In some diabetic circles the mere mention of the word carbohydrates can send off massive internal alarms. However, it may be possible that certain carbs may actually be beneficial once you understand how they deliver blood sugar to your system.
There are many carbs that flood your system with excess blood glucose. This can be especially difficult for diabetics, which is why there tends to be an intentional shift away from carbs in most instances.
The good news is there may be carb alternatives that can assist in the management of blood glucose due to their ability to act in a time released way. For instance plain white bread delivers carbs quickly to your system while dark whole-grained breads deliver valuable fiber while minimizing the potential of glucose overload due to carbs.
Interestingly pasta may actually better for you than rice when it comes to carbs simply because rice provide a quick release of blood glucose that can overload your system. Pasta may still not be the absolute best alternative, but you can offset this struggle by electing to use whole-wheat pasta that provides an incredible alternative low in glucose.
Sometimes those who aren’t diabetic tend to believe that it is sugar that causes the majority of problems for those who have diabetes. The truth is the carbs found in candy are the real culprit. There needs to be a distinction between sugar and blood glucose. Sugar doesn’t automatically become blood sugar. It is excess carbs that create the excess blood glucose. As far as fruit is concerned the worst offender in high carbs is watermelon. This is important to note simply because most dietitians will suggest fruit is something a diabetic can have within a regulated diet.
In those who are either not diabetic or prediabetic the role of carbs can play an important role in determine how best to eat for the greatest long-term benefits. It simply makes sense for all of us to work at keeping blood sugars from spiking, and one of the best ways to manage this is through education.
For those wanting to get a better handle on their glycemic index it just makes sense to work at regulating a diet that aids in digestion and long-term health.
For those who have diabetes it makes sense to follow a low-glycemic diet, Research indicates there is a decreased reliance on medication for those who follow such a management plan.
One of the most violent carb offenders is the potato. These white starch filled veggies add an immediate boost to your glycemic index and can leave you feeling a little sluggish.
Soluble fiber can be a great friend to the diabetic if for no other reason than the fiber is useful in the digestion of carbohydrates. Again, there are carbs that may be acceptable to eat, and added fiber can further reduce the impact of carbs.
If all of this seems to be a bit too much you need to know that it is knowledge that can allow you to not only understand the disease of diabetes, but also the opportunity to mitigate the damage and bring a better sense of order to your personally directed self management care.
Following this advice could result in a decrease in the instance of diabetes, heart disease as well as aiding in weight reduction goals.
 Gary Hall Jr. was born in 1974 from Cincinnati, Ohio. He is an Olympic swimmer that has competed and won several medals. Hall has competed in the last three Olympic swimming competitions. He has won a total of 10 medals for his efforts. His family is accomplished in the Olympics as well. Several members of the family have won medals throughout the years. Hall has various American honors including the Humanitarian Award in 2004.
Gary Hall Jr. was born in 1974 from Cincinnati, Ohio. He is an Olympic swimmer that has competed and won several medals. Hall has competed in the last three Olympic swimming competitions. He has won a total of 10 medals for his efforts. His family is accomplished in the Olympics as well. Several members of the family have won medals throughout the years. Hall has various American honors including the Humanitarian Award in 2004.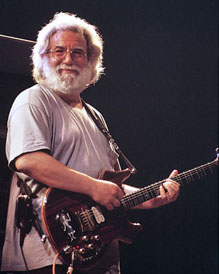 Jerry Garcia is most famous for his works with the Grateful Dead. He was an American music icon. Born Jerome John Garcia in 1942 from San Francisco, California, he took the world by storm. His band was recording and performing their songs for over three decades. Garcia is remembered for his works that include “I’ll Take a Melody”, “The Wheel” and “Might as Well”. His large base of fans called themselves “Deadheads.” Jerry Garcia rocked right up until the end; he died in 1995 of a heart attack. He was only 53 years old.
Jerry Garcia is most famous for his works with the Grateful Dead. He was an American music icon. Born Jerome John Garcia in 1942 from San Francisco, California, he took the world by storm. His band was recording and performing their songs for over three decades. Garcia is remembered for his works that include “I’ll Take a Melody”, “The Wheel” and “Might as Well”. His large base of fans called themselves “Deadheads.” Jerry Garcia rocked right up until the end; he died in 1995 of a heart attack. He was only 53 years old. George C. Scott was an incredible dramatic performer. He was born in 1927, a native from Wise, Virginia. His original goal in life was to become a writer. Scott was in the Marines and when he was discharge he went to college for a little while. However, he become intrigued with drama and shortly thereafter left to pursue his dreams. Scott began on Broadway, and then became a motion picture star. Some of his most remember works include “Patton”, “They Might be Giants” and “The Hindenburg”. During his career he received several awards including the Academy Award for Best Actor. Yet Scott called the awards ceremony a “parade.” In 1971, when they expected him to come for his Oscar, he did not come forward to get the award. Scott did not appear for the show. George C. Scott died in 1999 of an abdominal aneurysm. He was 72 years old.
George C. Scott was an incredible dramatic performer. He was born in 1927, a native from Wise, Virginia. His original goal in life was to become a writer. Scott was in the Marines and when he was discharge he went to college for a little while. However, he become intrigued with drama and shortly thereafter left to pursue his dreams. Scott began on Broadway, and then became a motion picture star. Some of his most remember works include “Patton”, “They Might be Giants” and “The Hindenburg”. During his career he received several awards including the Academy Award for Best Actor. Yet Scott called the awards ceremony a “parade.” In 1971, when they expected him to come for his Oscar, he did not come forward to get the award. Scott did not appear for the show. George C. Scott died in 1999 of an abdominal aneurysm. He was 72 years old. Waylon Jennings was born in 1937 from Littlefield, Texas. He is an icon in the American country music industry. Jennings had a distinctive voice that everyone recognized. In his early career, he played bass for Buddy Holly. When the plane crashed that took several talented musicians Buddy Holly, The Big Bopper and Richie Valens, Jennings was booked on that plane ride. However, at the last minute, he gave his seat to The Big Bopper. Jennings may be remembered mostly for his work on the “Dukes of Hazard”. He was the voice of the announcer as well as sung the theme song. Jennings had several hit songs including “MacAuthur Park”, “Delia’s Gone” and “Just to Satisfy You”. Among his achievements, he has won various awards, including “Lifetime Achievement Award”, “Male Vocalist of the Year” and “Album of the Year”. Jennings was elected to the Country Music Hall of Fame in 2001 and inducted to Hollywood’s Rockwall in 2006. Waylon Jennings died in 2002 from diabetes
Waylon Jennings was born in 1937 from Littlefield, Texas. He is an icon in the American country music industry. Jennings had a distinctive voice that everyone recognized. In his early career, he played bass for Buddy Holly. When the plane crashed that took several talented musicians Buddy Holly, The Big Bopper and Richie Valens, Jennings was booked on that plane ride. However, at the last minute, he gave his seat to The Big Bopper. Jennings may be remembered mostly for his work on the “Dukes of Hazard”. He was the voice of the announcer as well as sung the theme song. Jennings had several hit songs including “MacAuthur Park”, “Delia’s Gone” and “Just to Satisfy You”. Among his achievements, he has won various awards, including “Lifetime Achievement Award”, “Male Vocalist of the Year” and “Album of the Year”. Jennings was elected to the Country Music Hall of Fame in 2001 and inducted to Hollywood’s Rockwall in 2006. Waylon Jennings died in 2002 from diabetes