 Bayer Contour USB Glucose Meter: Throughout history, diabetes management has been a difficult process, mainly due to the monitors that record blood glucose results. Through time products have obtained a higher status and even made testing easier and less painful than before. However, it was not until Bayer’s revolutionary portable blood glucose monitor showed up in the medical market that things really began to change.
Bayer Contour USB Glucose Meter: Throughout history, diabetes management has been a difficult process, mainly due to the monitors that record blood glucose results. Through time products have obtained a higher status and even made testing easier and less painful than before. However, it was not until Bayer’s revolutionary portable blood glucose monitor showed up in the medical market that things really began to change.
That was nearly forty years ago that Bayer’s first portable blood glucose monitor hit the medical market. With every year, due to technical advances, medical machinery gets better and better. Thanks to Bayer, the future of healthy, fast and effective diabetes management is easier than ever due to the new Contour USB Meter.
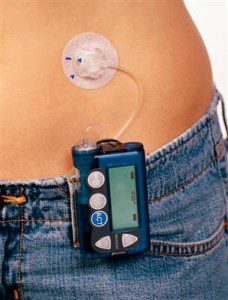
In today’s world, nearly everything can be completed on the computer. Due to the internet, much more can be done such paying your bills, doing some Christmas shopping and even in some areas do some grocery shopping. Now, with the Contour USB Meter, you can also keep your diabetes tests on your computer with simple and easy technology that comes with your monitor.
The new Contour USB Meter has a plug and play feature which makes connecting to your computer fast and easy, even for those who are not quite as computer savvy as others. Easy GlucoFacts Deluxe Software makes the install simple and fast as well.
With the new Contour USB Meter, you can keep up with your diabetes management by setting up a reminder for yourself. In today’s world, it is easy to get lost in the fast paced rush of work, school and others events that keep us all busy. With the Contour USB Meter, you’ll get a reminder to let you know when it is time to test and thanks to the 2,000 storage capacity unit, you will always have your results handy.
When you have more time available, make sure you use the insights that will help your doctor to understand how you were feeling when you took your blood sugar. You can mark your test results as “sick” or “stress”, you can add whatever you would like to describe the way you are feeling at the moment.
The new Contour USB meter is a great adaptable, small portable blood sugar monitor that is perfect for the on-the-go lifestyle.
 There are over 24 million Americans who have been diagnosed with diabetes and more than 25 percent of them will develop some sort of foot
There are over 24 million Americans who have been diagnosed with diabetes and more than 25 percent of them will develop some sort of foot 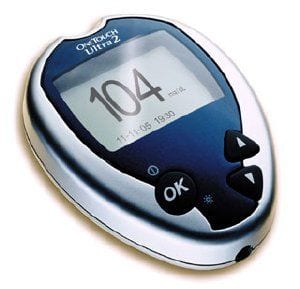 Through
Through 

 The SUPERVALU family of grocery stores (including Acme®, Albertsons®, Cub Foods®, Farm Fresh®, Jewel-Osco®, Shaw’s/Star Market™, Shop ‘n Save®, and Shoppers Food & Pharmacy®) has just launched “living healthy with my diabetes™,” a program that will feature a variety of year-round resources, as well as special limited-time services starting Nov. 7 through Nov. 20 during American Diabetes Month.
The SUPERVALU family of grocery stores (including Acme®, Albertsons®, Cub Foods®, Farm Fresh®, Jewel-Osco®, Shaw’s/Star Market™, Shop ‘n Save®, and Shoppers Food & Pharmacy®) has just launched “living healthy with my diabetes™,” a program that will feature a variety of year-round resources, as well as special limited-time services starting Nov. 7 through Nov. 20 during American Diabetes Month. Better Choices, Better Health, the new online version of Stanford University’s Chronic Disease Self Management Program (CDSMP). This new program is free for people in seven pilot states, thanks to a grant from The Atlantic Philanthropies.
Better Choices, Better Health, the new online version of Stanford University’s Chronic Disease Self Management Program (CDSMP). This new program is free for people in seven pilot states, thanks to a grant from The Atlantic Philanthropies. He sings, he dances and he can act. His name is Ben Vereen and he’s a diabetic. This star of stage and screen has taken his story to the people, and the people are listening.
He sings, he dances and he can act. His name is Ben Vereen and he’s a diabetic. This star of stage and screen has taken his story to the people, and the people are listening.