 Diabetic Blindness Could Be Prevented By Statin: A popular drug known as Statin (brand name, Lipitor) may help diabetic patients who are suffering from blindness, suggests a New University of Georgia study.
Diabetic Blindness Could Be Prevented By Statin: A popular drug known as Statin (brand name, Lipitor) may help diabetic patients who are suffering from blindness, suggests a New University of Georgia study.
Over 26 million people in America have been diagnosed with diabetes and diabetes retinopathy is the leading cause of blindness in adults. Diabetic retinopathy usually begins to happen when a patient has had diabetes for 10-15 years. Currently, no FDA-approved oral treatments can be found for those suffering from diabetic retinopathy and surgery is very painful and very expensive.
A study led by lead author Azza El-Remessy, an assistant professor in the University Of Georgia College Of Pharmacy, used diabetic rats to perform statin tests on. They found that the statins prevented free radicals in the retina from killing nerves, which are essential in maintaining vision.
With uncontrolled and excessive glucose, the introduction of free radicals becomes a huge problem. When free radicals appear in the retina, the eye releases a protein called pro-nerve growth factor. This factor matures into a nerve growth factor in an attempt to protect the retinal nerves. The free radicals generated by diabetes however, prevent this growth from happening, which ultimately leads to impaired neuronal function.
By using the rates and isolated retinal cells displayed in high glucose, El-Remessy and colleagues found that the drug atovastation blocked the formation of free radicals in the retina. Due to the blockage, pro-nerve growth factor was successfully able to mature into the nerve growth factor and preserved the neurons in the retina.
El-Remessy said, “It removed the break on the pro-form nerve growth factor to develop into its mature form,” she said. The drug was orally administered to rats in doses proportional to levels given to human patients with cardiovascular problems.
El-Remessy and her colleagues also found that a component within green tea called epicathecin is also helpful in the prevention of adverse affects on the pro-nerve growth factor in the retina. It will not affect the maturing from pro-nerve growth factor to nerve growth factor, but it regulates a receptor used by the pro-nerve growth factor that sends a signal to kill the neuron.
“We are still getting the same result, that we are preventing neuronal death and restoring neuronal function, but just in a different way,” said El-Remessy.
This study found great theoretical treatments for the eye, but it also was helpful for the rest of the body as well, which are continuously affected by diabetes.
“Diabetic patients need to protect the nerves beyond vision. El-Remessy stated.
El-Remessy study does not end her; she hopes to find treatment for other parts of the body dealing with the imbalance of pro-nerve growth factor as well. “If proNGF accumulates in the eyes in diabetes, I can imagine that it accumulates in the nerve endings in the skin, in the foot, in the hand and in the brain… everywhere,” she said.
This study was backed by the American Heart Association, which is making a difference from those suffering from diabetes.
 Chicago’s home town band, Ovrevolt, is hosting a fund raiser on May 6th at Real Time Sports Bar in St. Charles, from 6pm-1am. Ovrevolt (pronounced Over-volt) has 2 goals, one is to produce dynamic high
Chicago’s home town band, Ovrevolt, is hosting a fund raiser on May 6th at Real Time Sports Bar in St. Charles, from 6pm-1am. Ovrevolt (pronounced Over-volt) has 2 goals, one is to produce dynamic high 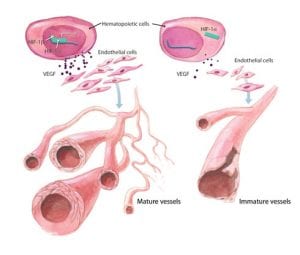 Diabetes: The Cause Of Blood Vessel Damage: More than 26 million people across American suffer from diabetes and by the time this year is up, another million will be diagnosed as well.
Diabetes: The Cause Of Blood Vessel Damage: More than 26 million people across American suffer from diabetes and by the time this year is up, another million will be diagnosed as well. Home Urine Test Measures
Home Urine Test Measures  Smoking Increased Among Youth With Diabetes: According to a new report from SEARCH Study Group, the number of young adults and children with diabetes who smoke has increased quite a bit, though health care providers are doing very little to encourage them to stop.
Smoking Increased Among Youth With Diabetes: According to a new report from SEARCH Study Group, the number of young adults and children with diabetes who smoke has increased quite a bit, though health care providers are doing very little to encourage them to stop. Researchers Look To Our Ancestors For Diabetic
Researchers Look To Our Ancestors For Diabetic  Popular Social Networking Websites And Diabetes: As the internet continues to grow, so does the need for social networking sites. Just under a half of U.S. adults who use the internet, use it to access social networking sites. Many social networking websites are focused on health but some are not as safe as they claim to be. Researchers at the Children’s Hospital Boston Informatics Program took a closer look through their evaluation of ten diabetic websites.
Popular Social Networking Websites And Diabetes: As the internet continues to grow, so does the need for social networking sites. Just under a half of U.S. adults who use the internet, use it to access social networking sites. Many social networking websites are focused on health but some are not as safe as they claim to be. Researchers at the Children’s Hospital Boston Informatics Program took a closer look through their evaluation of ten diabetic websites. Diabetes Affects Patients’ Spouses: Diabetes is a hard disease to manage and so many people are being diagnosed with the disease that it is becoming even harder and for far too many,
Diabetes Affects Patients’ Spouses: Diabetes is a hard disease to manage and so many people are being diagnosed with the disease that it is becoming even harder and for far too many,  Why Do Some Diabetics Never Encounter
Why Do Some Diabetics Never Encounter  Controlling Blood Sugar Levels Through
Controlling Blood Sugar Levels Through