 Study on Liraglutide (Victoza) Could Help Type 1 Diabetics: The University of Buffalo conducted an observation study in regards to the use of liraglutide, an injectable medication that is now used to treat only Type 2 diabetes, and how it might help Type 1 diabetics in achieving the very best blood sugar levels possible. This was a small study, and only a larger study that is now planned by the University of Buffalo might show that this could lead to better treatment for Type 1 diabetics. If this proves to be true, then this could be the newest treatment for Type 1 diabetics since the discovery of insulin back in the 1920s. The results of this study will eventually be in print and available in the European Journal of Endocrinology. This study received accolades at the annual meeting of the Endocrine Society in Boston. This study at University of Buffalo was headed by Paresh Dandona, a Professor of Medicine in the School of Medicine and Biomedical Sciences and was the senior author of the study.
Study on Liraglutide (Victoza) Could Help Type 1 Diabetics: The University of Buffalo conducted an observation study in regards to the use of liraglutide, an injectable medication that is now used to treat only Type 2 diabetes, and how it might help Type 1 diabetics in achieving the very best blood sugar levels possible. This was a small study, and only a larger study that is now planned by the University of Buffalo might show that this could lead to better treatment for Type 1 diabetics. If this proves to be true, then this could be the newest treatment for Type 1 diabetics since the discovery of insulin back in the 1920s. The results of this study will eventually be in print and available in the European Journal of Endocrinology. This study received accolades at the annual meeting of the Endocrine Society in Boston. This study at University of Buffalo was headed by Paresh Dandona, a Professor of Medicine in the School of Medicine and Biomedical Sciences and was the senior author of the study.
Approximately 23.6 million Americans have some form of diabetes, either Type 1 (the more serious and more difficult to control) or Type 2. The number of people with Type 2 diabetes is higher than those with Type 1, and a many number of people with Type 2 diabetes can manage their disease through diet, exercise and oral medication, or with the injectable liraglutide.
With Type 1 diabetes the only form of treatment is through insulin that must be injected. The insulin pump is now available, but this too involves the injection of insulin into the body.
The study showed that liraglutide (Victoza) along with insulin helped control blood sugar much better for tighter Type 1 diabetes management. Liraglutide, or also known as Victoza, is an acylated human glucagon-like peptide-1 (GLP-1) receptor agonist.
An A1C test is a blood test that is taken by diabetics approximately every three months by their physician. This A1C test result tells the physician and the patient how well they have controlled their blood sugar levels over those past months. If the A1C test is below 7, this is considered the best. If their A1C is higher than 7, then they know they need to take steps to better control their blood sugar levels, because the more out of control the blood sugar levels are, the more likely it is for severe complications to arise down the road. These complications include, but are not limited to, vision loss, kidney failure, and heart disease.
This was an unfunded study and was an analysis of data and was conducted at Kaleida Health’s Diabetes-Endocrinology Center of Western New York.
The study involved 14 Type 1 diabetic patients whose hemoglobin A1C levels were under the preferred “7.” In the study, these patients were deemed well controlled diabetics. Even though they were considered well controlled, even these patients had fairly wide swings in their blood sugar levels, some from 150 mg/dl to 250 mg/dl, and sometimes even higher than 250 mg/dl. So though deemed well controlled, they still had periods when their blood sugar level was too high for comfort.
With the addition of liraglutide to their insulin, these patients showed that they had fewer occasions when their blood sugar levels were too high, as well as a lessening in the amount of insulin they were injecting. A decrease in appetite was also noted.
Within a matter of days of the addition of liraglutide to their insulin, a positive result was seen. When the liraglutide was discontinued, their blood sugar levels again rose at times to higher levels than desired. This indicated that it was the addition of liraglutide that created the better controlled blood sugar levels.
More research is needed to understand the mechanics of the improvements in blood sugar levels with the addition of liraglutide to insulin, but it is thought that with the addition of liraglutide to insulin there is a decrease in the post-meal glucagon, which is the hormone that causes the increase in blood sugar levels in Type 1 diabetics.
With this further research, the researchers plan a multicenter study of patients with Type 1 diabetes and hopefully find more information on how the liraglutide suppresses the glucagon that raises the blood sugar levels to an unsafe level.
These patients took liraglutide for periods of one week to 24 weeks. There were 14 adult patients with Type 1 diabetes.
Hopefully, this new research that is planned will be expanded quickly and help even more in the care of Type 1 diabetes in the control of their blood sugar levels, an everyday battle for many people.
 Can eating 37 strawberries a day lessen diabetes
Can eating 37 strawberries a day lessen diabetes 
 Tom Martinez, Facebook And A Donor: Back in June of 2011, famous quarterback coach Tom Martinez announced on his Facebook page that his
Tom Martinez, Facebook And A Donor: Back in June of 2011, famous quarterback coach Tom Martinez announced on his Facebook page that his 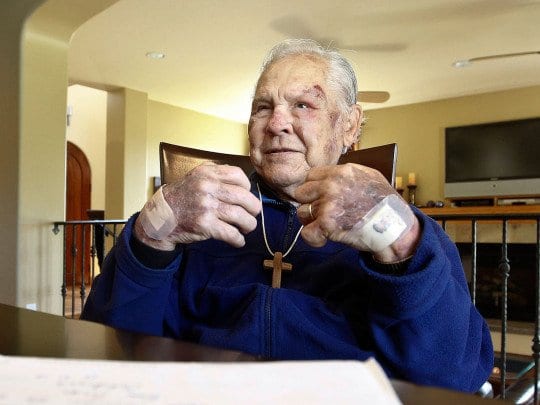
 New Discoveries Made in Conquering
New Discoveries Made in Conquering  High-Fat Diet
High-Fat Diet  Oil Refining Helping Researchers With New Tools For Type 1 Diabetes: In order to control blood sugar, engineering researchers from the Rensselaer Polytechnic Institute are merging automation techniques from oil refining in order to create a closed-loop
Oil Refining Helping Researchers With New Tools For Type 1 Diabetes: In order to control blood sugar, engineering researchers from the Rensselaer Polytechnic Institute are merging automation techniques from oil refining in order to create a closed-loop  HbA1C Results Prove Inaccurate For Dialysis Patients: According to a new study at Wake Forest Baptist Medical Center, a test known as the golden standard long-term glucose monitoring test proved to be less valuable in patients who are on dialysis.
HbA1C Results Prove Inaccurate For Dialysis Patients: According to a new study at Wake Forest Baptist Medical Center, a test known as the golden standard long-term glucose monitoring test proved to be less valuable in patients who are on dialysis. Master Gene Found To Cause Obesity And Diabetes: According to a study led by a team of King’s College London and the University of Oxford researchers, a “master regulator” gene is being named the culprit of high cholesterol levels and type 2 diabetes in the body.
Master Gene Found To Cause Obesity And Diabetes: According to a study led by a team of King’s College London and the University of Oxford researchers, a “master regulator” gene is being named the culprit of high cholesterol levels and type 2 diabetes in the body.