 Apple Peels, Diabetes and Muscle Wasting: You might not want to peel that apple before eating it, let alone put an apple peel down the garbage disposal or in the trash container under the sink.
Apple Peels, Diabetes and Muscle Wasting: You might not want to peel that apple before eating it, let alone put an apple peel down the garbage disposal or in the trash container under the sink.
Apple peels contains a good dose of ursolic acid. Ursolic acid is a natural compound found in apple peels called pentcyclic triterpenoid and helps to burn fat and build muscle. In a recent study in which mice were used, apple peel was shown to lower blood sugar levels, cholesterol and triglycerides. Ursolic acid is also known as malol, prunol, urson, 3-B-hydroxy-urs-12-en-28-oic acid.
This study was conducted by Dr. Chris Adams, an endocrinologist and senior author of the study for the University of Iowa. The study showed that the ursolic acid found in apple peels could be helpful with the wasting away of muscles that occurs in certain diseases, and also possibly help with metabolic disorders like diabetes. The study results were published in the June 2011 issue of Cell Metabolism.
From the information from his study, Dr. Adams stated, “We found that it actually promoted the growth of muscle, so the mice got bigger muscles and actually got stronger. We can measure mouse strength with a little machine called a grip strength meter.” He added, “It didn’t have any harmful effect on the kidneys or liver or anything like that which makes sense because it’s a natural compound that we actually eat.”
The mice that received the ursolic acid became leaner and had lower blood sugar levels, cholesterol and triglycerides. Further testing will be needed before it is determined that the same positive results will prove to be true for humans.
The muscle-building aspect of the ursolic acid would be beneficial in the treatment of the infirmed and elderly.
Also, it is not known whether the amount of ursolic acid that is consumed on a daily basis by humans would produce the same results.
Ursolic acid is found in apple peels, but it is also found in other plants, including bilberries, cranberries, hawthorn, prunes, elder flowers, lavender, oregano, thyme and peppermint. Ursolic acid has already been recognized as an inhibitor of various types of cancer cells.
Ursolic acid is currently used by the cosmetic industry in the manufacture of cosmetics in its topical form due to its anti-tumor (skin cancer) properties.
Type 1 and Type 2 diabetes diagnoses are growing in number each year. Every little piece of new information garnered that could help in the treatment of these conditions helps all those with these numerous conditions.
In the meantime, we might want to do what we are always told: Eat your fruits and veggies.
 Zebrafish, Zinc and Diabetes: Zinc is an important trace mineral that people need to stay healthy. Only iron is in stronger form in the body than zinc. Zinc’s highest concentrations are found in the prostate gland and sperm of men, the red and white blood cells, the retinas of the eyes, the liver and the
Zebrafish, Zinc and Diabetes: Zinc is an important trace mineral that people need to stay healthy. Only iron is in stronger form in the body than zinc. Zinc’s highest concentrations are found in the prostate gland and sperm of men, the red and white blood cells, the retinas of the eyes, the liver and the  Study Shows Life Expectancy Longer Now For Type 1 Diabetics:
Study Shows Life Expectancy Longer Now For Type 1 Diabetics:  New Study On Clogged Carotid Arteries And Type 1 Diabetes: Atherosclerosis of the carotid arteries is a buildup of plaque in either the right or left carotid artery, located at the sides on the neck going up to the head. These carotid arteries supply oxygenated blood to the head and neck and are vital for survival. When either of these arteries becomes clogged with plaque, this blood flow to the head and neck can be stopped, and a stroke or a mini-stroke occurs, which could impact a person’s life forever. Usually, the buildup of plaque in the carotid arteries occurs over a period of time.
New Study On Clogged Carotid Arteries And Type 1 Diabetes: Atherosclerosis of the carotid arteries is a buildup of plaque in either the right or left carotid artery, located at the sides on the neck going up to the head. These carotid arteries supply oxygenated blood to the head and neck and are vital for survival. When either of these arteries becomes clogged with plaque, this blood flow to the head and neck can be stopped, and a stroke or a mini-stroke occurs, which could impact a person’s life forever. Usually, the buildup of plaque in the carotid arteries occurs over a period of time. New Drug Delivery Mechanism For
New Drug Delivery Mechanism For 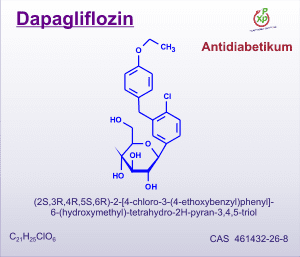 New Drug Potential from Squibb and AstraZeneca for Type 2 Diabetes:
New Drug Potential from Squibb and AstraZeneca for Type 2 Diabetes: 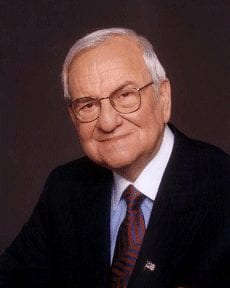 Lee Iacocca has donated over $30 million to diabetes research seeking a cure for the disease, which can lead to debilitating and fatal
Lee Iacocca has donated over $30 million to diabetes research seeking a cure for the disease, which can lead to debilitating and fatal  Islet Cell Transplant is Cure for Type 1 Diabetes for Lady in Scotland: Kathleen Duncan, a resident of Scotland, no longer has to take injections of
Islet Cell Transplant is Cure for Type 1 Diabetes for Lady in Scotland: Kathleen Duncan, a resident of Scotland, no longer has to take injections of 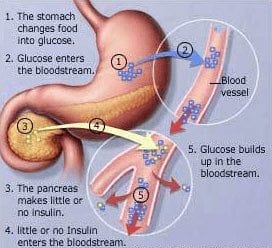 Hopes for an
Hopes for an  Lab-Created Blood Vessels Helping Dialysis Patients: Imagine having to stop your
Lab-Created Blood Vessels Helping Dialysis Patients: Imagine having to stop your