 Physicist Aaron Keller and his colleagues at the Helmholtz-Zentrum Dresden-Rossendorf in Germany and at Aarhus University in Denmark have reported a significant advancement in the possibility of treatment for Type 2 diabetes and Alzheimer’s disease. The researchers are studying amyloids, or clumps of proteins that form in the body, which seem to be closely related to the development of these diseases. If doctors could prevent these clumps from forming they might have an effective defense against diabetes and Alzheimer’s.
Physicist Aaron Keller and his colleagues at the Helmholtz-Zentrum Dresden-Rossendorf in Germany and at Aarhus University in Denmark have reported a significant advancement in the possibility of treatment for Type 2 diabetes and Alzheimer’s disease. The researchers are studying amyloids, or clumps of proteins that form in the body, which seem to be closely related to the development of these diseases. If doctors could prevent these clumps from forming they might have an effective defense against diabetes and Alzheimer’s.
Amyloids form on the surfaces of different types of cells, namely the cells of the pancreas in diabetes and the brain in Alzheimer’s. Physicians currently do not have imaging technology that can view these processes as they occur, but Adrian Keller and his colleagues are working to recreate these processes artificially in tests at the Interdisciplinary Nanoscience Center in Aarhus, known as “iNano.”
Recreating the processes on an artificial surface is difficult because of the properties of the cell surfaces in organisms. Cells can be hydrophilic or hydrophobic, which means they either attract water or repel water, respectively.
Adrian Keller has used mica crystal to recreate the amyloid-forming process. He has configured the surface of the mica so that positively-charged atoms of argon gas are only able to slightly penetrate into the surface of the material. “This chemically activates the surface without significantly changing the roughness,” said Keller of the first step of the process. The roughness of the surface would also influence the possibility that amyloids could form there.
Next, Keller places the processed mica into boxes and stores them in the lab for several weeks. While stored away, the surface of the mica adsorbs hydrocarbons in the air around it. The surface of the mica gradually becomes hydrophobic instead of hydrophilic; after about three months, the mica is totally hydrophobic (water repellent).
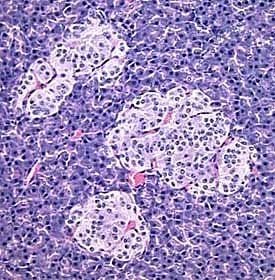
Keller conducts experiments during these three months. He places amylin, a small protein, on the mica. This protein is also produced by certain pancreatic cells along with insulin. When an organism develops Type 2 diabetes, its body’s reaction to insulin becomes less effective. The organism’s blood sugar elevates and the pancreas produces more insulin and amylin in response to the increased blood sugar. Some of the amylin proteins assume a concave “bowl” shape and influence nearby amylin proteins to follow suit.
The misshapen amyloid proteins begin to stick together, forming amyloids. These clumps destroy pancreatic cells and reduce insulin production, which causes the other cells to ramp up their own insulin produciton. The cycle continues and the organism’s insulin production mechanism can be devastated.
In Keller’s experiments, the amylins clump together on the surface of the mica according to the nature of the crystal’s surface. If the experiment has just been started and the surface is still hydrophilic, the amylin proteins form clusters called “fibrils.” However, if the mica has been gathering hydrocarbons and the surface is becoming hydrophobic, the amylins increasingly form clumps called “oligomers.” Both oligomers and fibrils work to destroy the surface of the cells, though they work through different mechanisms. In either case, when the clumps form on pancreatic cells, they inhibit insulin production.
Keller’s experiments have allowed researchers to view the creation of amyloid clumps for the first time in history. This new technology may pave the way for researchers to develop methods of preventing the clumping process and thus preventing diabetes and Alzheimer’s.
 Tampa Bay Rays outfielder Sam Fuld made the day of one six-year-old boy when he visited Andrew Cordovez in an examination room. Fuld had one special connection with the young boy: they both have Type 1 diabetes.
Tampa Bay Rays outfielder Sam Fuld made the day of one six-year-old boy when he visited Andrew Cordovez in an examination room. Fuld had one special connection with the young boy: they both have Type 1 diabetes. Mannkind (MKND) stock rose more than 20%, showing increased investor confidence after the fledgling pharmaceutical company confirmed that it has received approval from the FDA for clinical trials on its key product. Mannkind received FDA clearance to conduct efficacy trials on a new inhaled
Mannkind (MKND) stock rose more than 20%, showing increased investor confidence after the fledgling pharmaceutical company confirmed that it has received approval from the FDA for clinical trials on its key product. Mannkind received FDA clearance to conduct efficacy trials on a new inhaled  Researchers at York University have discovered a new
Researchers at York University have discovered a new  Patients suffering with Type 2 diabetes are commonly prescribed a combination of
Patients suffering with Type 2 diabetes are commonly prescribed a combination of  Fat Levels Higher in Thin Children” width=”290″ height=”249″ />A study conducted by Children’s Hospital Boston and the Joslin Diabetes Center has revealed that levels of “brown fat,” a healthy type of fat that appears in children, increase in puberty and then decrease after. The study also showed that thinner children have higher levels of brown fat. The study was published in the Journal of Pediatrics.
Fat Levels Higher in Thin Children” width=”290″ height=”249″ />A study conducted by Children’s Hospital Boston and the Joslin Diabetes Center has revealed that levels of “brown fat,” a healthy type of fat that appears in children, increase in puberty and then decrease after. The study also showed that thinner children have higher levels of brown fat. The study was published in the Journal of Pediatrics. The Journal of Sexual Medicine recently published a new study demonstrating that weight loss in men with Type 2 diabetes is more than just a healthy choice. It also improves sexual health, increasing erectile function and desire while lowering the risk of developing urinary tract symptoms.
The Journal of Sexual Medicine recently published a new study demonstrating that weight loss in men with Type 2 diabetes is more than just a healthy choice. It also improves sexual health, increasing erectile function and desire while lowering the risk of developing urinary tract symptoms. The smell of that hamburger or steak (unprocessed meat) on the backyard grill is tantalizing, but we all know that we’re not supposed to have too much of it simply because it’s not great for our health for a number of reasons, to include the susceptibility to type 2 diabetes. But, it’s now known that that hotdog (processed meat) lying beside that hamburger on the grill might be a little bit worse for your health than the burger or steak, including your susceptibility to type 2 diabetes.
The smell of that hamburger or steak (unprocessed meat) on the backyard grill is tantalizing, but we all know that we’re not supposed to have too much of it simply because it’s not great for our health for a number of reasons, to include the susceptibility to type 2 diabetes. But, it’s now known that that hotdog (processed meat) lying beside that hamburger on the grill might be a little bit worse for your health than the burger or steak, including your susceptibility to type 2 diabetes. The heavy competition present in the modern
The heavy competition present in the modern  Boston Therapeutics has filed an abbreviated new drug application (or ANDA) with the Food and Drug Administration. The new drug appears in the form of chewable
Boston Therapeutics has filed an abbreviated new drug application (or ANDA) with the Food and Drug Administration. The new drug appears in the form of chewable