 Researchers at UCLA demonstrated that the common over-the-counter dietary supplement gamma-Aminobutyric acid (also known as GABA) may aid in inhibiting the development of insulin resistance and glucose tolerance, two conditions that are known to be precursors to the development of both Type 2 diabetes and metabolic syndrome.
Researchers at UCLA demonstrated that the common over-the-counter dietary supplement gamma-Aminobutyric acid (also known as GABA) may aid in inhibiting the development of insulin resistance and glucose tolerance, two conditions that are known to be precursors to the development of both Type 2 diabetes and metabolic syndrome.
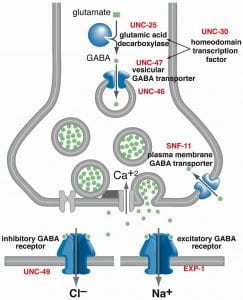
In the preclinical study, researchers gave GABA to mice that were obese, had developed insulin resistance, and were in the early stages of Type 2 diabetes. GABA is a naturally-produced compound similar to amino acids that plays an important role in inhibitory processes in the central nervous system of all mammals. When the researchers gave GABA to the mice, they found that the compound worked to suppress the inflammatory immune responses that are associated with the development of Type 2 diabetes.
According to the investigation’s authors, GABA aided in preventing progression of Type 2 diabetes; in addition, it improved insulin sensitivity and glucose tolerance in the mice, even after they had already developed Type 2 diabetes. They also identified regulatory immune cells that play a role in GABA’s inhibition of inflammation.
The research team commented that future studies on the effects of GABA on conditions associated with Type 2 diabetes could provide new medications based on the compound that treat metabolic syndrome and Type 2 diabetes related to obesity.
GABA has become popular in recent years as a dietary supplement promising everything from weight loss to muscle gain to reduced anxiety and depression to better sleep. Since GABA is an inhibitor, it is frequently promoted as a compound that stops excessive brain activity, allowing the individual to relax and eliminate anxiety. “It’s the brakes of your brain. It stops activity,” says Karl Doghramji, M.D., director of the Sleep Disorders Center at Thomas Jefferson University Hospital in Philadelphia.
It is thought that GABA reduces the effects of glutamate, a neurochemical that increases agitation and excitement. By taking GABA, individuals may be able to silence their overactive thoughts and, for example, get a better night’s sleep. Deficiencies in GABA levels are thought to cause a lack of “delta” sleep — the “deep” stage of sleep that begins about 45 minutes after one falls asleep. Lacking this type of sleep could be damaging to an individual’s mental health, according to Dr. Doghramji; those suffering with depression, anxiety, and other disorders often don’t get enough delta sleep.
Research shows that long-term deficiencies in delta sleep can cause more serious problems. One in three people who suffer with recurrent insomnia has some kind of psychiatric disorder, while 25% of those individuals also have anxiety problems.
However, there isn’t sufficient evidence yet to determine whether GABA supplements have an effect on improving sleep patterns and moods. “We just don’t have any data on them. We do not know how much GABA is really in the supplement or the product’s purity. There are no studies backing up the claims made by the supplement manufacturers.”
According to the New York University Langone Medical Center, there is no evidence that GABA supplements are effective in reducing symptoms from anxiety “presumably because the substance itself cannot pass the blood-brain barrier and enter the central nervous system.” Because they do not actually affect brain chemistry, GABA supplements are most likely ineffective in treating mood disorders, though they may still have some utility in treating hypertension.
 Having insects liquefy and digest the dead tissue from your wounds might not be the most appealing idea, but a research team in Hawaii has done just that — using maggots to clean infected and dead tissue from wounds in diabetics — with very positive results.
Having insects liquefy and digest the dead tissue from your wounds might not be the most appealing idea, but a research team in Hawaii has done just that — using maggots to clean infected and dead tissue from wounds in diabetics — with very positive results. A recent preliminary study suggests that people taking the prescription drugs
A recent preliminary study suggests that people taking the prescription drugs  A small retrospective study recently presented at the annual meeting of the European Society for the Study of Diabetes has demonstrated that elevated accumulation of
A small retrospective study recently presented at the annual meeting of the European Society for the Study of Diabetes has demonstrated that elevated accumulation of  According to a recent study published in the October 1 issue of the “The American Journal of Cardiology,” percutaneous coronary intervention (or PCI) of chronic total occlusions (CTOs) is associated with reduced mortality in people with diabetes and can also reduce the need for coronary artery bypass grafting.
According to a recent study published in the October 1 issue of the “The American Journal of Cardiology,” percutaneous coronary intervention (or PCI) of chronic total occlusions (CTOs) is associated with reduced mortality in people with diabetes and can also reduce the need for coronary artery bypass grafting. A study recently reported in the journal “Pediatrics” has demonstrated that pregnant women with well-managed diabetes may not be at increased risk of giving birth to preterm infants or infants with very low birth weight.
A study recently reported in the journal “Pediatrics” has demonstrated that pregnant women with well-managed diabetes may not be at increased risk of giving birth to preterm infants or infants with very low birth weight.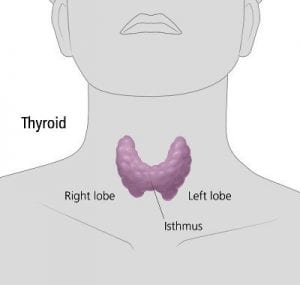 Previous research has suggested the possibility that having diabetes could increase an individual’s lifetime risk of also developing thyroid cancer. A new report, however, has solidified that claim, demonstrating that the association holds true for retirement-age Americans. The findings were published in the journal “Thyroid.”
Previous research has suggested the possibility that having diabetes could increase an individual’s lifetime risk of also developing thyroid cancer. A new report, however, has solidified that claim, demonstrating that the association holds true for retirement-age Americans. The findings were published in the journal “Thyroid.” Patients who have been diagnosed with Type 2 diabetes can demonstrate elevated levels of glucose and glycated hemoglobin (HbA1c) even 10 years before their actual diagnosis, according to Esther van’t Riet, Ph.D., with the Department of Epidemiology and Biostatistics at VU University Medical Center in Amsterdam. Dr. van’t Riet presented the information at a poster session at the 47th annual meeting of the European Association for the Study of Diabetes (EASD). According to Dr. van’t Riet, individuals demonstrate moderate increases and then rapid increases in the few years prior to the diagnosis of diabetes, with increases in Hba1c often preceding elevated glucose.
Patients who have been diagnosed with Type 2 diabetes can demonstrate elevated levels of glucose and glycated hemoglobin (HbA1c) even 10 years before their actual diagnosis, according to Esther van’t Riet, Ph.D., with the Department of Epidemiology and Biostatistics at VU University Medical Center in Amsterdam. Dr. van’t Riet presented the information at a poster session at the 47th annual meeting of the European Association for the Study of Diabetes (EASD). According to Dr. van’t Riet, individuals demonstrate moderate increases and then rapid increases in the few years prior to the diagnosis of diabetes, with increases in Hba1c often preceding elevated glucose. Doctors have long extolled the health values of getting eight hours of sleep every night. Add another benefit to the list: new research shows that getting eight and a half hours of sleep every night could reduce the risk of developing Type 2 diabetes in teenagers who are obese. The findings were published in the journal “Diabetes Care.”
Doctors have long extolled the health values of getting eight hours of sleep every night. Add another benefit to the list: new research shows that getting eight and a half hours of sleep every night could reduce the risk of developing Type 2 diabetes in teenagers who are obese. The findings were published in the journal “Diabetes Care.”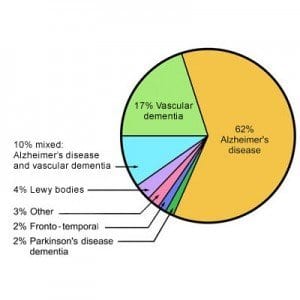 A longitudinal study conducted in Japan has shown that risk of dementia increases when glucose levels swing out of control, especially directly after
A longitudinal study conducted in Japan has shown that risk of dementia increases when glucose levels swing out of control, especially directly after