 A study recently published in the journal “Cancer” has discovered that therapy with the drug tamoxifen — an oral medication used in women with breast cancer — is linked to a significant increase in development of diabetes in older survivors of breast cancer.
A study recently published in the journal “Cancer” has discovered that therapy with the drug tamoxifen — an oral medication used in women with breast cancer — is linked to a significant increase in development of diabetes in older survivors of breast cancer.
The study was headed by Lorraine L. Lipscombe, M.D., with the Women’s College Hospital in Toronto. Dr. Lipscombe’s team studied 14,360 women over the age of 65 who had been diagnosed with early-stage breast cancer and had survived. The women had received treatment for breast cancer with tamoxifen therapy. The study used data collected from 1996 to 2006; the patients who were diagnosed with diabetes through March 31, 2008 were matched with control subjects who had not developed diabetes. The research team adjusted for other risk factors and compared the risk of developing diabetes in participants who received tamoxifen and aromatase inhibitor therapy compared to women who were not treated with those drugs.
According to the study’s findings, 10 percent of the patients received a diagnosis of diabetes over a mean follow-up of 5.2 years. Women who were currently receiving tamoxifen therapy had a significantly higher chance of developing diabetes (1.24 adjusted odds ratio) over women who were not being treated with tamoxifen. Treatment with aromatase inhibitors, on the other hand, was found not to be linked to an increased risk of developing diabetes.
“Current tamoxifen therapy is associated with an increased incidence of diabetes in older breast cancer survivors. These findings suggest that tamoxifen treatment may exacerbate an underlying risk of diabetes in susceptible women,” wrote the authors of the study.
Tamoxifen, marketedd as Nolvadex, Istubal, and Valodex in the U.S., is an orally-administered tablet that disrupts the female body’s production of estrogen, which is known to promote breast cancer in women. Tamoxifen binds to the estrogen receptor proteins, effectively blocking additional binding at the site that would cause cancerous growth. Tamoxifen is approved by the FDA for the treatment of breast cancer and other types of cancer and has been used for over 30 years in the treatment of early-stage breast cancer.
The drug has also been used to reduce the risk of breast cancer in women who are at increased risk of developing the disease. It works by blocking the effects of estrogen on breast cancer cells with estrogen receptor-positive proteins, preventing the growth of the cancerous cells. However, the medication is only useful in treating cancer cells that are specifically estrogen receptor-positive. Doctors must determine whether the tumor will respond to tamoxifen treatment before prescribing the drug.
Tamoxifen therapy is known to be associated with several serious side effects, including stroke, blood clots, uterine cancer, and cataracts. It may also cause symptoms similar to menopause such as hot flashes, irregular menstrual periods, headaches, nausea, and fatigue. Though tamoxifen therapy does cause blood clots or stroke in a small number of women, the chances of developing such complications are similar to those associated with estrogen replacement therapy.
Additional adverse side effects associated with tamoxifen therapy include an increased risk of thromboembolism and fatty liver as well as mental effects such as reduced cognition and degraded memory, though memory loss with tamoxifen therapy is not as severe as with aromatase inhibitor therapy. Tamoxifen has also been associated with reduced libido.
However, not all the side effects of tamoxifen therapy are negative; it is known to improve bone health, especially in women, by inhibiting osteoclasts and preventing osteoporosis.
 Doctors and scientists have long known that people with Type 2 diabetes are at an increased risk of developing certain types of cancer. Until recently, the mechanisms behind the link between the two diseases have been unclear to medical professionals.
Doctors and scientists have long known that people with Type 2 diabetes are at an increased risk of developing certain types of cancer. Until recently, the mechanisms behind the link between the two diseases have been unclear to medical professionals. A large meta-analysis of
A large meta-analysis of  A study recently conducted by researchers at Glasgow University in Scotland found that men develop Type 2 diabetes faster than women do in terms of weight gain. The study’s findings showed that Type 2 diabetes occurred in men at a lower body mass index (BMI) than it did in women. The research could provide the reasoning behind higher rates of diabetes among men throughout many areas of the world.
A study recently conducted by researchers at Glasgow University in Scotland found that men develop Type 2 diabetes faster than women do in terms of weight gain. The study’s findings showed that Type 2 diabetes occurred in men at a lower body mass index (BMI) than it did in women. The research could provide the reasoning behind higher rates of diabetes among men throughout many areas of the world. A recent study suggests that significant accumulation of calcium buildup in coronary arteries could be a signal of an impending heart attack in individuals who have metabolic syndrome and diabetes.
A recent study suggests that significant accumulation of calcium buildup in coronary arteries could be a signal of an impending heart attack in individuals who have metabolic syndrome and diabetes. A recent review of past research has confirmed that individuals with diabetes are at an increased risk of developing colon cancer. However, scientists aren’t sure why the connection exists or what can be done to lower the risk. The findings were reported in the American Journal of Gastroenterology.
A recent review of past research has confirmed that individuals with diabetes are at an increased risk of developing colon cancer. However, scientists aren’t sure why the connection exists or what can be done to lower the risk. The findings were reported in the American Journal of Gastroenterology. A research team at the John G. Rangos Sr. Research Center at Children’s Hospital of Pittsburgh of UPMC and the University of Pittsburgh School of Medicine has discovered a molecular pathway responsible for regulating management of
A research team at the John G. Rangos Sr. Research Center at Children’s Hospital of Pittsburgh of UPMC and the University of Pittsburgh School of Medicine has discovered a molecular pathway responsible for regulating management of 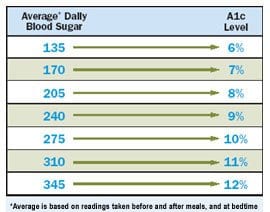 A large United States-backed study recently discovered that lowering blood glucose levels in older individuals with diabetes was helpful in preserving brain volume in the patients but did not help in mitigating the effects of memory loss. The findings were published in the journal “Lancet Neurology.”
A large United States-backed study recently discovered that lowering blood glucose levels in older individuals with diabetes was helpful in preserving brain volume in the patients but did not help in mitigating the effects of memory loss. The findings were published in the journal “Lancet Neurology.” Diabetics looking to network with other patients online have a variety of options, including the availability of a doctor to answer questions, who reviews the material posted on the website, and which companies are allowed advertising space on the website.
Diabetics looking to network with other patients online have a variety of options, including the availability of a doctor to answer questions, who reviews the material posted on the website, and which companies are allowed advertising space on the website. A study published in the September 26 issue of the journal “Archives of Internal Medicine” has demonstrated that diabetics are healthier when they visit their doctors frequently. The patients involved with the study who saw their primary care physicians once every 1 to 2 weeks had a better chance of achieving their clinical goals than patients who saw their doctors less frequently.
A study published in the September 26 issue of the journal “Archives of Internal Medicine” has demonstrated that diabetics are healthier when they visit their doctors frequently. The patients involved with the study who saw their primary care physicians once every 1 to 2 weeks had a better chance of achieving their clinical goals than patients who saw their doctors less frequently.