 Findings from a new study suggest that people who have previously suffered from kidney stones could have a higher risk of developing Type 2 diabetes later in life. Previous research has shown that kidney stones appear to be more common in individuals who have diabetes, but scientists have been unsure as to whether the reverse is true as well.
Findings from a new study suggest that people who have previously suffered from kidney stones could have a higher risk of developing Type 2 diabetes later in life. Previous research has shown that kidney stones appear to be more common in individuals who have diabetes, but scientists have been unsure as to whether the reverse is true as well.
The new study was conducted at Taipei Medical University in Taiwan. Dr. Herng-Ching Lin and his colleagues analyzed medical records from over 94,000 Taiwanese adults and found that individuals with a history of kidney stones demonstrated a 30 percent increase in their chance of being diagnosed with diabetes over five years than were individuals who did not have kidney stones.
The medical records showed that out of 23,000 adults who had received treatment for kidney stones, 12.4 percent later developed Type 2 diabetes. Of the 70,700 adults who did not have kidney stones, only 9.6 percent developed diabetes.
According to the researchers, some of the overlap between kidney stones and diabetes could be caused by common risk factors between the two conditions. Older age and obesity are commonly listed among the risk factors for both.
However, the researchers accounted for age, obesity, and other health risks when investigating the relationship between kidney stones and diabetes, and they still found that individuals with kidney stones had a one-third higher risk of developing diabetes.
The researchers stated that they were uncertain about the mechanism that causes the relationship. They hypothesized, however, that both kidney stones and diabetes could be caused by some of the same processes.
Kidney stones are formed due to the presence of excessive amounts of crystal-forming substances, such as uric acid, calcium, and oxalate. The minerals cannot be diluted by the available fluid and form small stones which typically do not cause long-term damage but can be very painful when they pass through the urine.
According ot Lin’s research team, there is evidence suggesting that insulin, the hormone responsible for regulating blood glucose levels, could be associated to the formation of kidney stones in some way. Previous research in both animals and humans has suggested that elevated insulin levels can alter the chemical composition of urine, making the formation of kidney stones more likely. Since Type 2 diabetes is associated with high insulin levels due to the body’s inability to use it correctly, the two conditions could be related through the actions of insulin.
Lin’s team noted that their own study had limitations, namely the fact that they used existing medical records—which can be inaccurate—to arrive at their findings. The researchers also did not have access to information about the diet, exercise habits, and family history of the conditions due to the lack of that information in the medical records. Such data could have helped the researchers determine the source of the association between kidney stones and diabetes.
According to the research team, it’s still possible that the formation of kidney stones could be a warning sign that the individual could have an increased risk of developing diabetes. Those who find themselves diagnosed with kidney stones may also benefit from making lifestyle changes that reduce the chances of developing diabetes, including eating a healthy diet and getting more exercise.
Previous research has showed that people with diabetes and insulin resistance have highly-acidic urine, which is a risk factor for developing kidney stones, and especially uric acid kidney stones.
 A new study suggests that doctors may be able to help diagnose diabetes and related warning signs through the use of a “muffin test.” The test would be a type of oral glucose tolerance test designed to identify diabetes and impaired glucose tolerance by analyzing the body’s ability to utilize glucose properly.
A new study suggests that doctors may be able to help diagnose diabetes and related warning signs through the use of a “muffin test.” The test would be a type of oral glucose tolerance test designed to identify diabetes and impaired glucose tolerance by analyzing the body’s ability to utilize glucose properly. Two former graduate students at MIT’s George R. Harrison Spectroscopy Laboratory have developed new spectrograph technology that could allow diabetics to monitor their blood glucose levels without pricking their fingers to draw blood for testing. Kong and Barman significantly reduced the size of the spectrograph, allowing the technology to be used in much more convenient spaces.
Two former graduate students at MIT’s George R. Harrison Spectroscopy Laboratory have developed new spectrograph technology that could allow diabetics to monitor their blood glucose levels without pricking their fingers to draw blood for testing. Kong and Barman significantly reduced the size of the spectrograph, allowing the technology to be used in much more convenient spaces. Researchers located in the United Kingdom say that levels of a hormone called B-type natriuretic peptide could have a role in reducing risk of Type 2 diabetes. The study was published online in the journal “PLoS Medicine.”
Researchers located in the United Kingdom say that levels of a hormone called B-type natriuretic peptide could have a role in reducing risk of Type 2 diabetes. The study was published online in the journal “PLoS Medicine.” The American Diabetes Association recently released a position statement which stated that, in helping young people transition into more responsible roles for managing their own diabetes, parents should gradually transfer the responsibilities associated with the disease to their children.
The American Diabetes Association recently released a position statement which stated that, in helping young people transition into more responsible roles for managing their own diabetes, parents should gradually transfer the responsibilities associated with the disease to their children.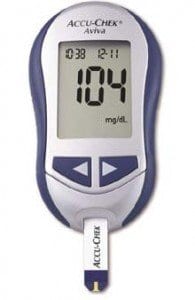 A recent investigation found that U.S. adults who have been diagnosed with diabetes are about two times more likely to contract hepatitis B infections. The findings prompted a recommendation to the Centers for Disease Control and
A recent investigation found that U.S. adults who have been diagnosed with diabetes are about two times more likely to contract hepatitis B infections. The findings prompted a recommendation to the Centers for Disease Control and  New research suggests that drinking less than a couple of glasses of water every day increases an individual’s risk of having elevated blood sugar levels in an unhealthy range.
New research suggests that drinking less than a couple of glasses of water every day increases an individual’s risk of having elevated blood sugar levels in an unhealthy range. A new kind of “ultrafast”
A new kind of “ultrafast” 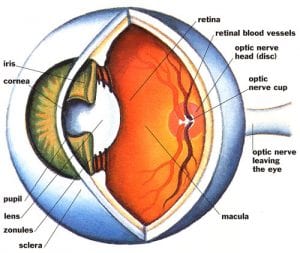 A recent study found that phacoemulsification, a process by which the internal lens of the eye is emulsified as a treatment for cataracts, does not affect intraocular pressure (IOP) in individuals who have diabetes. The findings were presented in a poster session at the American Academy of Opthalmology 2011 Annual Meeting, and they contradict previous research on the subject of phacoemulsification’s effects on intraocular pressure.
A recent study found that phacoemulsification, a process by which the internal lens of the eye is emulsified as a treatment for cataracts, does not affect intraocular pressure (IOP) in individuals who have diabetes. The findings were presented in a poster session at the American Academy of Opthalmology 2011 Annual Meeting, and they contradict previous research on the subject of phacoemulsification’s effects on intraocular pressure. A new study conducted in Canada suggests that women who have been recently diagnosed with diabetes are more likely to also be diagnosed with breast cancer.
A new study conducted in Canada suggests that women who have been recently diagnosed with diabetes are more likely to also be diagnosed with breast cancer.