 Recently, researchers have found that fruit flies, who are overeating in the area of carbohydrates and protein not only have a shorter life span but they gain weight and develop insulin resistance as well.
Recently, researchers have found that fruit flies, who are overeating in the area of carbohydrates and protein not only have a shorter life span but they gain weight and develop insulin resistance as well.
Insulin resistance is a common problem that is linked Type 2 diabetes; poor diet and obesity are also linked to it as well. In the United States alone, more than 25 million people have been diagnosed with type 2 diabetes and another million more will be diagnosed by this time next year. It is a growing disease, despite the strides made from researchers to find a successful cure.
Biologists from the Southern Methodist University in Dallas now say they have developed a tool that could help researchers to understand the disease more.
Researchers have always used mice, rats and other animals when it comes to diabetic genetic and metabolic changes. Now, they are turning to a different species, fruit flies. Recently, fruit flies have been used to investigate an array of human disease such as cancer and Alzheimer’s disease.
Fruit flies have two advantages when it comes to the investigation of these diseases, they don’t live very long and they are inexpensive. Through investigation, an insulin-resistant fruit fly was created in a lab at the Southern Methodist University in Dallas. Feeding fruit flies a high diet in nutrients accomplished it, reported Johannes H. Bauer, the principal investigator for the investigation. It is the same process, which happens in humans, overeating to the point of obesity and then developing insulin resistance.
Since the same process is seen between humans and fruit flies, they can serve as an efficient model for studying type 2 diabetes.
Bauer states, “We learned that by manipulating the nutrients of fruit flies, we can make them insulin resistant. With this insulin-resistant model we can now go in with pinpoint precision and study the molecular mechanisms of insulin resistance, as well as drug treatments for the condition, as well as how to treat obesity, how to block insulin resistance and how metabolic changes from a specific diet develop. The possibilities are endless.”
Carbohydrates and protein are two overfeeding diets that cause insulin resistance. Insulin itself is produced from the pancreas and is a hormone that communicates with our cells, which allows for the absorption of glucose. Glucose is necessary because it helps the brain to function, makes repairs to our bodies and allows us to grow and move.
During the investigation, researchers implemented their testing strategies two separate ways. One, by feeding fruit flies, carbohydrates and two, by feeding fruit flies, protein. Researchers believed that the fruit flies that were fed carbohydrates would develop insulin resistance but were surprised to find that the fruit flies fed the protein diet appeared to develop insulin resistance at a quicker rate. Bauer said, “ Carb-loaded flies gain weight. Protein-loaded flies gain and then lose weight. So the two diets have exactly opposite effects on metabolism. But too much of either one of them causes insulin resistance. That surprised us.”
 Diabetes affects more than 25 million people in the United States and plagues its victims with serious medical conditions such as
Diabetes affects more than 25 million people in the United States and plagues its victims with serious medical conditions such as  What do these three conditions have in common after a woman is over 60 years of age?
What do these three conditions have in common after a woman is over 60 years of age?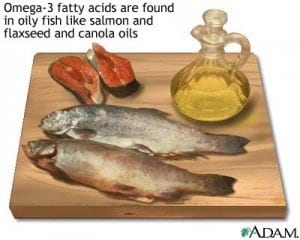 New findings from the Alpha Omega Trial suggest that low-dose omega-3 fatty acid supplementation could play a role in preventing ventricular arrhythmia-related events in patients who have both diabetes and a history of myocardial infarction.
New findings from the Alpha Omega Trial suggest that low-dose omega-3 fatty acid supplementation could play a role in preventing ventricular arrhythmia-related events in patients who have both diabetes and a history of myocardial infarction.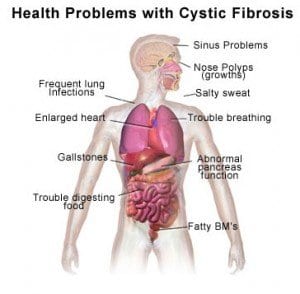 In addition to Type 1 and Type 2 diabetes, there is another variant of the disease: cystic fibrosis-related diabetes. It differs in some important ways from Type 1 and Type 2 diabetes and it requires different treatment methods.
In addition to Type 1 and Type 2 diabetes, there is another variant of the disease: cystic fibrosis-related diabetes. It differs in some important ways from Type 1 and Type 2 diabetes and it requires different treatment methods. New research conducted at the University of Glasgow, Scotland, suggests that thrombolytic drugs—also called “clot-busting” drugs due to their use in dissolving blood clots—improve outcomes in patients who have suffered from strokes, even when they have a past history of stroke or diabetes. In fact, outcomes were similar to those demonstrated by patients who had experienced neither stroke nor diabetes.
New research conducted at the University of Glasgow, Scotland, suggests that thrombolytic drugs—also called “clot-busting” drugs due to their use in dissolving blood clots—improve outcomes in patients who have suffered from strokes, even when they have a past history of stroke or diabetes. In fact, outcomes were similar to those demonstrated by patients who had experienced neither stroke nor diabetes. A new study found that an enzyme called IKKbeta was linked to increased metabolism in lab mice. When researchers engineered the mice to express the IKKbeta enzyme in their
A new study found that an enzyme called IKKbeta was linked to increased metabolism in lab mice. When researchers engineered the mice to express the IKKbeta enzyme in their  The latest statistics of the International Diabetes Federation predict that diabetes rates will continue to rise in the coming years. By 2030, the IDF predicts, 552 million people could have the disease, or at least one in 10 adults worldwide.
The latest statistics of the International Diabetes Federation predict that diabetes rates will continue to rise in the coming years. By 2030, the IDF predicts, 552 million people could have the disease, or at least one in 10 adults worldwide. Diabetics around the world are familiar with the routine of blood glucose testing that requires a prick on the finger to draw blood. Though the inconvenience of drawing blood is a small price to pay for accurate blood sugar control, some diabetics require several tests a day and the frequent pricks can be tiring.
Diabetics around the world are familiar with the routine of blood glucose testing that requires a prick on the finger to draw blood. Though the inconvenience of drawing blood is a small price to pay for accurate blood sugar control, some diabetics require several tests a day and the frequent pricks can be tiring. Medtronic, Inc., the world’s largest medical technology company, recently announced that it received approval from the U.S. Food and Drug Administration for its Investigational Device Exemption (IDE) in conducting a pivotal clinical trial in the ASPIRE study, an investigation of the in-home efficacy of the Low Glucose Suspend feature of Medtronic’s MiniMed Paradigm
Medtronic, Inc., the world’s largest medical technology company, recently announced that it received approval from the U.S. Food and Drug Administration for its Investigational Device Exemption (IDE) in conducting a pivotal clinical trial in the ASPIRE study, an investigation of the in-home efficacy of the Low Glucose Suspend feature of Medtronic’s MiniMed Paradigm