Over two million DNA markers per person were analyzed and two genes were found (AFF3 and ERBB4) which were increases for kidney disease.
 Two genes have been discovered by a group of international researchers that increases the risk of developing diabetes that is associated with kidney disease.
Two genes have been discovered by a group of international researchers that increases the risk of developing diabetes that is associated with kidney disease.
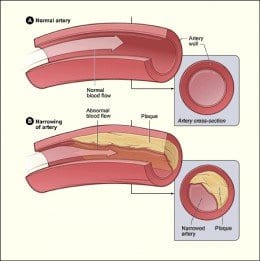
Kidney disease is a common problem when it comes to the complications of diabetes and the disease typically leads to both strokes and heart attacks. Diabetic kidney disease is known world-wide as the leading cause of kidney failure in which a kidney transplant or dialysis is used as treatment.
Researchers led a study from the Queen’s University Belfast, University College Dublin, Harvard University and the University of Helsinki in order to find significant evidence about genes associated with both diabetes and kidney disease.
The study was congratulated by Professor Bernie Hannigan, Director of HSC R&D who said, “This research consortium is tremendously productive. Their dedicated work will immediately benefit patient management and in the longer term can lead to new treatments with both health and economic impacts. Such international research collaboration can result in gains for all partners involved.”
This study is the largest of its kind, 4,750 patients with diabetic kidney disease and nearly 7,000 patients with long-standing diabetes (with no kidney disease) were recruited for the study.
A principal of the study, Professor Peter Maxwell of Queen’s University said, “Currently available drugs cannot cure the kidney failure but may slow its progression. Knowing which patients are most at risk of kidney complications will be helpful in managing their diabetes.”
Over two million DNA markers per person were analyzed and two genes were found (AFF3 and ERBB4) which were increases for kidney disease.
Professor Catherin Godson, lead investigator of the UCD group stated, “These new research findings are very important as they help accelerate development of new and effective therapies.”





 Two genes have been discovered by a group of international researchers that increases the risk of developing diabetes that is associated with
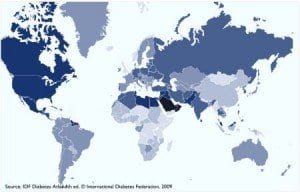
Two genes have been discovered by a group of international researchers that increases the risk of developing diabetes that is associated with  Diabetes is a common problem all around the world and while many studies have shown great strides in helping to calm the disease, at best, there are still many more tests and studies that are yet to be discovered that may in fact cure diabetes once and for all.
Diabetes is a common problem all around the world and while many studies have shown great strides in helping to calm the disease, at best, there are still many more tests and studies that are yet to be discovered that may in fact cure diabetes once and for all.