 What Is Gestational Diabetes: Many have heard the term “Gestational Diabetes”, but have never really been sure what it was. The word gestational has to do with pregnancy while the word diabetes in this case refers to insulin levels that are not sufficient to manage blood glucose. Unlike Type 1 or Type 2 diabetes this type generally goes away following delivery.
What Is Gestational Diabetes: Many have heard the term “Gestational Diabetes”, but have never really been sure what it was. The word gestational has to do with pregnancy while the word diabetes in this case refers to insulin levels that are not sufficient to manage blood glucose. Unlike Type 1 or Type 2 diabetes this type generally goes away following delivery.
The development of this condition during pregnancy appears to be influenced significantly by hormone release typical in pregnancy. Women who develop gestational diabetes will typically do so in the final trimester of pregnancy.
The American Diabetics Association (ADA) indicates there are about, “135,000 cases of gestational diabetes in the United States each year.”
Normally glucose is used by the body to create energy, but in the case of gestational diabetes insulin does not provide the support the body needs for the conversion process. This deficit results in a condition called hypoglycemia. What this essentially means is your body has more glucose than it needs and struggles to either use or eliminate it without the aid of sufficient insulin.
It is important to know that diabetes during pregnancy requires managed care just like Type 1 or Type 2 diabetes. Without proper care and attention the mother could unintentionally be placing their unborn child at risk.
Two Scenarios
Tanya is six months pregnant. Her doctor just informed her that she has gestational diabetes. A managed care plan was offered and Tanya took advantage of the proactive steps needed to protect herself and her child. With proper care Tanya delivered a beautiful and healthy baby and is on the road to personal recovery.
Kelly heard that gestational diabetes takes care of itself following pregnancy so she didn’t think it was important to modify her personal care plan. After all, she only had three months left before the baby was due. How much harm could happen in three months?
What’s Going on Inside?
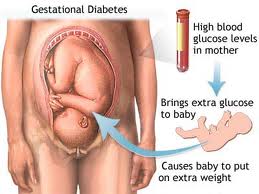
Your baby is connected to you via the umbilical cord. When you have high blood glucose so does your baby. When your body is working overtime to manufacture insulin so is your baby’s. When your child can’t produce enough insulin to take care of the flood of blood glucose it will store that glucose as fat. The end result is a chubby baby that may have long-term trouble getting rid of their baby fat and may experience respiratory issues following delivery.
The ADA indicates, “Babies with excess insulin become children who are at risk for obesity and adults who are at risk for type 2 diabetes.”
By working with a primary care physician during pregnancy to manage your blood glucose you are offering improved health to your unborn child.
Long-term Results
By working with your health care provider to manage your blood glucose and then continuing positive lifestyle changes following pregnancy you can give your child a healthy start while minimizing the real potential of developing Type 2 diabetes later in life. This is true for both you and your child. This is why gestational diabetes should not be viewed as only a temporary problem that will go away after pregnancy. It is a condition that essentially places a billboard in your life asking for personal change.
Virtually all health care providers will suggest a three-prong approach to successful long-term management.
- Effective personal weight management.
- A plan for regular physical activity
- Informed choice and discipline in food selection.
Estimates indicate gestational diabetes will affect 3-8% of the population. Your physician will generally check for this condition prior to your third trimester.