 An estimated 25.8 million Americans have diabetes, and seven million of those may not be diagnosed has been recorded by the National Diabetes Information Clearinghouse.
An estimated 25.8 million Americans have diabetes, and seven million of those may not be diagnosed has been recorded by the National Diabetes Information Clearinghouse.
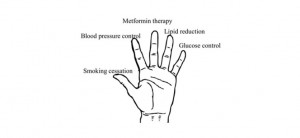
A new approach to teaching about diabetes could be more helpful to doctors to explain to their patients what a diabetic treatment looks like. The new approach is called “lending a hand” and it uses the fingers of an open hand to depict a diabetes intervention from thumb to pinky, in order of the most beneficial treatment from smoking cessation (thumb), to blood pressure control, to metformin therapy to lipid reduction, to glucose control (pinky).
The “lending a hand” approach helps doctors to help their patients to learn about the best treatments for diabetes by re-prioritizing treatment goals and to show that glycemic control is not the only primary intervention, as ,medical science once believed.
People who have been diagnosed with Type 2 diabetes will benefit more from smoking cessation and that is why it’s the first one on the list, according to senior author Allen Shaughnessy, Pharm.D., M.Med.Ed., professor of family medicine at Tufts University School of Medicine and fellowship director of the Tufts University Family Medicine Residency Program at Cambridge Health Alliance who stated, “Glycemic control is stuck in people’s minds as the primary goal of treatment, but evidence has existed since the 1970s that other interventions are of greater benefit.”
Shaughnessy and colleagues tested illustrated through the “lending a hand” approach the paradigm shift in treatment priorities. They wanted to show that one finger (smoking cessation) proved more beneficial in healing that another finger (glucose control) while also keeping within the guidelines of American Diabetes Association and the European Association for the Study of Diabetes.
Shaughnessy reported, “Some degree of glycemic control is necessary to prevent symptoms. It’s just that the return on investment is low when we try to push patients with diabetes to get their blood glucose as close as possible to normal.”
Deborah Erlich, M.D., M.Med.Ed., assistant professor at TUSM, assistant family medicine clerkship director, and program director of the new Carney Family Medicine Residency, a TUSM affiliate said, “Our aim in proposing “lending a hand” is to communicate the most beneficial interventions patients can make to reduce their symptoms and risk of death from diabetes complications. But this model requires a shift in thinking away from the outdated idea that glucose reduction is most important, which may be a challenge.”
“Working to control blood glucose while not addressing the other risk factors first is like rearranging deck chairs on the Titanic. The ship’s going down,” concluded author David Slawson, M.D., professor and vice chair of the department of family medicine, director of the Center for Information Mastery, and director of the family medicine fellowship at University of Virginia School of Medicine.