 A recent study found that phacoemulsification, a process by which the internal lens of the eye is emulsified as a treatment for cataracts, does not affect intraocular pressure (IOP) in individuals who have diabetes. The findings were presented in a poster session at the American Academy of Opthalmology 2011 Annual Meeting, and they contradict previous research on the subject of phacoemulsification’s effects on intraocular pressure.
A recent study found that phacoemulsification, a process by which the internal lens of the eye is emulsified as a treatment for cataracts, does not affect intraocular pressure (IOP) in individuals who have diabetes. The findings were presented in a poster session at the American Academy of Opthalmology 2011 Annual Meeting, and they contradict previous research on the subject of phacoemulsification’s effects on intraocular pressure.
The poster session detailed the findings of a retrospective chart review which studied the effects of phacoemulsification on patients with diabetes as well as those who had not been diagnosed with the disease. Elevated intraocular pressure in diabetics is a significant issue for doctors since it can precede future loss of vision.
The study was presented by Lisa Park, M.D., and was conducted by a research team at the New York University Langone Medical Center in New York City. Dr. Park’s team analyzed intraocular pressure data from 146 diabetic and non-diabetic patients who underwent cataract phacoemulsification. Measurements of IOP were taken before the procedure, then 1 day, 1 week, and 1 month after the procedure. Patients who did not have diabetes demonstrated significantly lower IOP at the 1 week and 1 month readings after the procedure (1.7mm Hg and 1.8mm Hg, respectively). However, IOP was not significantly different in patients with diabetes at the 1 week or 1 month marks (0.4mm Hg and 0.1mm Hg, respectively). There was a significant difference between diabetics and non-diabetics at the 1 week and 1 month marks (12.7 versus 15.mm Hg at 1 week; 12.6 versus 15.5mm Hg at 1 month).
According to the researchers, the findings demonstrate that diabetics do not benefit from the lowering of intraocular pressure as a result of the phacoemulsification procedure that non-diabetics do.
“Our results show that postoperative IOP is significantly different between diabetic and nondiabetic patients, and that the pressure-lowering effect [seen in previous studies] is not demonstrable in the diabetic population,” they wrote.
According to Dr. Park, the findings may demonstrate that the effects of phacoemulsification on intraocular pressure have simply not received much research.
“Not a lot has been known about postoperative IOP in diabetics. Information has been more anecdotal. A number of factors can be involved in IOP. Our study is different, in that we focused exclusively on IOP and diabetes,” said Dr. Park.
If further research proves demonstrably that cataract surgery does not lower intraocular pressure in diabetics, it could point to difficulties related to vision that extend beyond cataracts. Dr. Park stated that the growing number of individuals with diabetes warrants additional research into methods of reducing intraocular pressure.
“With the population aging and diabetes growing to epidemic proportions, we are going to need to focus more on this segment of the population. Management to reduce IOP after surgery along with management of inflammatory reactions could be done,” she said.
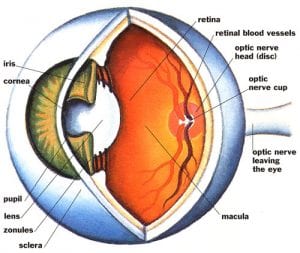
Patients with diabetes are advised to schedule regular visits with an ophthalmologist, as the high blood glucose levels associated with diabetes can cause swelling in the eyes that affect vision. Cataracts, or clouding of the eye, are especially common in individuals with diabetes: they form earlier in life for diabetics and they progress more quickly, causing impaired vision. The lens is unable to focus light and vision is reduced. Common treatments for cataracts include surgery and glasses or contact lens to correct vision.