Scientists as the Gladstone Institutes are looking into the power of regenerative medicine. Through the use of animal models, scientists have developed a technique that shows skin cells creating insulin-producing cells. The long term goal of this new study is to assist people who have been diagnosed with Type 1 diabetes to find a way to treat their diabetes without the use of life-long injections.
Type 1 diabetes happens when there has been a mass destruction of B-cells, which is a type of cell that resides in the pancreas and produces a hormone called insulin. When the body does not produce enough insulin, the human organs began to have difficulty in absorbing sugars like glucose, from the blood stream.
For years, scientists have been using insulin injections as a treatment for Type 1 diabetes however; scientists want to go above and beyond an insulin injection. They want to replace the missing B-cells instead. It is not as simple as taking them from one part of the body and placing them in another. Instead, stem cell technology has become a way to make them.
“The power of regenerative medicine is that it can potentially provide an unlimited source of functional, insulin-producing ß-cells that can then be transplanted into the patient. But previous attempts to produce large quantities of healthy ß-cells — and to develop a workable delivery system — have not been entirely successful. So we took a somewhat different approach.” said Dr. Ding, a professor at the University of California, San Francisco (UCSF).
While this does seem like a great step in the medical world, scientists are learning that they have to take a step backwards in the life cycle of a cell. This happens because once a cell has matured; it can be difficult to make more.
First, skin cells, which are called fibroblasts, are collected from laboratory mice. The fibroblasts are then treated with a cocktail mixture of molecules and reprogramming factors, which transforms them into endoderm-like cells, which are cells that are found in the early embryo stages, which eventually mature into major organs, such as the pancreas.
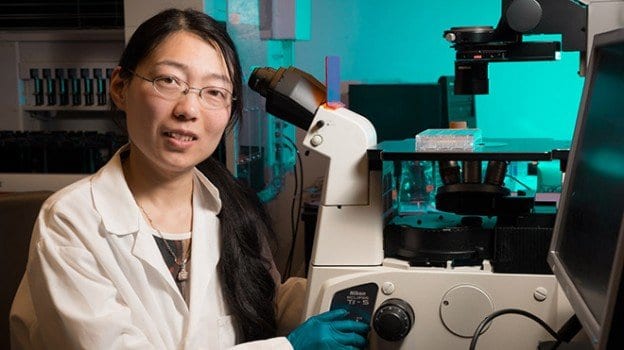
“Using another chemical cocktail, we then transformed these endoderm-like cells into cells that mimicked early pancreas-like cells, which we called PPLC’s,” “Our initial goal was to see whether we could coax these PPLC’s to mature into cells that, like ß-cells, respond to the correct chemical signals and — most importantly — secrete insulin. And our initial experiments, performed in a petri dish, revealed that they did.” said lead author and Gladstone Postdoctoral Scholar, Ke Li, PhD.
After the initial study, the researchers wanted to see if the same thing would occur in actual real life animals. Therefore, they transplanted PPLC’s into mice which had been modified to have hyperglycemia.
Dr. Li states, “Importantly, just one week post-transplant, the animals’ glucose levels started to decrease gradually approaching normal levels and when we removed the transplanted cells, we saw an immediate glucose spike, revealing a direct link between the transplantation of the PPLC’s and reduced hyperglycemia.”
After eight weeks, the mice appeared to have dramatic changes. The researchers noted that the mice had fully functional, insulin-secreting B-cells.
“These results not only highlight the power of small molecules in cellular reprogramming, they are proof-of-principle that could one day be used as a personalized therapeutic approach in patients.” said Dr. Ding.
Matthias Hebrok, PhD, one of the study’s authors and director of the UCSF Diabetes Center states, “I am particularly excited about the prospect of translating these findings to the human system. Most immediately, this technology in human cells could significantly advance our understanding of how inherent defects in ß-cells result in diabetes, bringing us notably closer to a much-needed cure.”