 Neural stem cells may someday be used to replace the beta cells of the pancreas that are destroyed by diabetes, according to a Japanese research team. The findings, which were published in a recent issue of the journal “EMBO Molecular Medicine,” demonstrate how the shortage of transplantable, donated beta cells could be overcome by using stem cells to regenerate an individual’s own beta cells.
Neural stem cells may someday be used to replace the beta cells of the pancreas that are destroyed by diabetes, according to a Japanese research team. The findings, which were published in a recent issue of the journal “EMBO Molecular Medicine,” demonstrate how the shortage of transplantable, donated beta cells could be overcome by using stem cells to regenerate an individual’s own beta cells.
Affecting over 200 million people around the world, diabetes is caused by decreased insulin production in the pancreas—specifically, in the beta cells of the pancreas. No cure for the disease exists today, so patients must rely on supplemental insulin treatment or other therapeutics to ensure that blood glucose levels remain regulated.
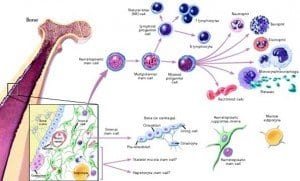
The research team was headed by Dr. Tomoko Kuwabara with the AIST Institute in Tsubuka, Japan. Dr. Kuwabara’s team focused developing new ways to control stem cell differentiation in humans, which would allow scientists to transplant stem cells and give them instructions to regrow any type of cell in the human body, such as pancreatic beta cells.
Dr. Kuwabara commented that since diabetes is caused by a lack of only one type of cell, it makes a good candidate for treatment with stem cells. “As diabetes is caused by the lack of a single type of cell the condition is an ideal target for cell replacement treatments,” he said. “However donation shortages of pancreatic beta cells are a major hurdle to advancing this treatment. So a safe and easy way of using stem cells for obtaining new beta cells has been long awaited.”
Dr. Kuwabara’s team used cells from the hippocampus and olfactory bulbs—regions of the brain that scientists can easily access to obtain transplantable cells. These brain cells do not normally produce insulin in the capacity that beta cells do. However, when the neuronal cells were transplanted into diabetic rats, they began to express important characteristics normally seen in the beta cells of the pancreas. They also began to produce more insulin, resulting in a decrease of average blood glucose levels. When the transplanted cells were removed, blood glucose levels increased, revealing that the cells were responsible for the positive changes. According to the research team, this method of transplanting brain cells into the pancreas could prove to be an effective treatment for diabetes that focuses on addressing the lack of beta cells rather than medicating insulin or blood glucose levels.
“The discovery of stem cells which have virtually unlimited self-renewal raises great expectations for their use in regenerative medicine,” wrote Onur Basak and Hans Clevers, who published a close up paper in the same issue of EMBO Molecular Medicine.
“The isolation and cultivation of stem cells as a renewable source of beta cells would be a major breakthrough,” they continued.
Basak and Clevers added: “Dr Kuwabara’s team found that transplanting neural stem cells directly into the pancreas can unleash their intrinsic ability to act as critical regulators of insulin production, and most importantly they demonstrated that the cells could be gained from a patient without the need for genetic manipulation.”
“Our findings demonstrate the potential value of neural stem cells for treating diabetes without gene transfer,” said Dr. Kuwabara. “This presents an original strategy to overcome the donor shortage which has hindered cell replacement therapy.”