 Diabetes: The Cause Of Blood Vessel Damage: More than 26 million people across American suffer from diabetes and by the time this year is up, another million will be diagnosed as well.
Diabetes: The Cause Of Blood Vessel Damage: More than 26 million people across American suffer from diabetes and by the time this year is up, another million will be diagnosed as well.
Damaged blood vessels are such a growing problem in diabetic patients that heart attacks, strokes and amputations are becoming more common daily. Thanks to the researchers at the Washington University School of Medicine in St. Louis, a significant mechanism is said to be the contributor to the damage of blood vessels in diabetic patients.
According to this study, mice have shown damage which involved two enzymes, fatty acid synthase (FAS) and nitric oxide synthase (NOS), which interacted in the cells that line the blood vessel walls.
Here is what Xiaochao Wei, Ph.D said, “We already knew that in diabetes there’s a defect in the endothelial cells that line the blood vessels. People with diabetes also have depressed levels of fatty acid synthase. But this is the first time we’ve been able to link those observations together.”
Wei is a postdoctoral research scholar in the lab of Clay F. Semenkovich, MD, the Herbert S. Gasser Professor of Medicine. He studied the mice which had been genetically engineered so that would make FAS in their tissue, which are the endothelial cells that line blood vessels. The mice began experiencing problems in their vessels, which was compared to the same problems animals experience when they have diabetes.
“It turns out that there are strong parallels between the complete absence of FAS and the deficiencies in FAS induced by lack of insulin and by insulin resistance.” stated Semenkovich
When comparing the FASTie mice to normal animals, even other mice, Semenkovich and Wei found out that mice without FAS could not make the substance that attaches nitric oxide synthase to the endothelial cells in blood vessels.
“We’ve known for many years that to have an effect, NOS has to be anchored to the wall of the vessel,” said Semenkovich. “Xiaochao discovered that fatty acid synthase preferentially makes a lipid that attaches to NOS, allowing it to hook to the cell membrane and to produce normal, healthy blood vessels.”
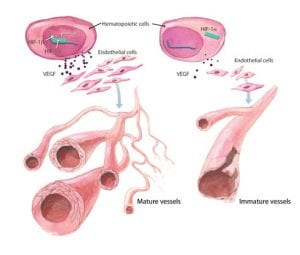
Throughout the study, the Fastie mice blood vessels grew leaky and even became injured and were not able to regenerate new blood vessel growth, in some cases.
The significant mechanism that attaches NOS to the endothelial cells is called palmitoylation. If it were not for the FAS, the mice would lose the NOS palmitoylation, which would make the mice incapable of NOS modification. It would not be able to attach to the endothelial cell membrane, causing major damage to the blood vessels.
In an explanation given by Semekovich, he says, “In animals that don’t have fatty acid synthase and normal nitric oxide synthase in endothelial cells, we saw a lot of leaky blood vessels. The mice also were more susceptible to the consequences of infection, and they couldn’t repair damage that occurred — problems that also tend to be common in people with diabetes.”
Trying different things during the study, researchers interrupted blood flow to the normal leg of a normal mouse and a FASTie mouse. Semenkovich states what happened, “”The control animals regained blood vessel formation promptly but that did not happen in the animals that were modified to be missing fatty acid synthase.”
Just because this is how it works in mice does not mean it will work the same in humans. So researchers looked toward human endothelial cells next. They found the same significant mechanism that was found in the mice.
“Our findings strongly suggest that if we can use a drug or another enzyme to promote fatty acid synthase activity, specifically in blood vessels, it might be helpful to patients with diabetes. We also have been able to demonstrate that palmitoylation of nitric oxide synthase is impaired in diabetes, and if we can find a way to promote the palmitoylation of NOS, even independent of fatty acid synthase, it may be possible to treat some of the vascular complications of diabetes.” Wei states.
According to the researchers, it shouldn’t matter if a person has type 1 diabetes and has become resistant to insulin or has type 2 diabetes
Semenkovich says “That’s one of the key findings. It won’t matter whether it’s an absence of insulin or resistance to insulin: both are associated with defects in FAS.”