 Window Tinting and Diabetic Retinopathy: Diabetic retinopathy is a disease of the retina of the eye and is a complication of the eye that is usually caused by either Type 1 or Type 2 diabetes, but most often Type 1. Type 1 diabetes is usually diagnosed in the young, those whose pancreas has stopped producing insulin, and the person is forced to take artificial insulin the remainder of their life in order to stay alive.
Window Tinting and Diabetic Retinopathy: Diabetic retinopathy is a disease of the retina of the eye and is a complication of the eye that is usually caused by either Type 1 or Type 2 diabetes, but most often Type 1. Type 1 diabetes is usually diagnosed in the young, those whose pancreas has stopped producing insulin, and the person is forced to take artificial insulin the remainder of their life in order to stay alive.
Diabetic retinopathy can lead to blood leaking into the retina from ruptured blood vessels, causing new, weaker blood vessels to form. Once these new vessels break, which can occur at any time, the blood leaks into the middle part of the eye in front of the retina and vision is altered. The bleeding can cause scar tissue, which can then cause the retina to become detached or cause a large rupture in any of the blood vessels, or cause a slow leaking of blood. These gradual events can lead to blindness, if not treated.
Diabetes is the leading cause of new blindness in adults from the age of 20 to the age of 74. This is a very strong reason to keep your diabetes under control as well as you can, and to also see an ophthalmologist annually so any signs of retinopathy can be addressed immediately.
With today’s modern technology, diabetic retinopathy can be treated through laser surgery. A laser is used to stop the growth of new and weaker blood vessels. But each time laser surgery is performed on the eye, a little of the vision is lost, and a little bit of sensitivity to the eyes might be noticed.
As well as some vision loss, there could be sensitivity to light – a flash from a camera going off in one’s face, bright sunlight when outside on a sunny day, even strong light coming in through the windows of the home. Looking at a computer screen for long hours can cause eye discomfort. Most of these situations can be taken care of by simply avoiding flashing from cameras, closing the blinds at home, wearing darkened sunglasses when outside, tilting the computer screen around so you can see a little better, even taking a break from the computer. Some people have chosen to have the windows in their homes tinted to decrease the amount of strong sunlight coming into the home.
When you are in your car, you can wear your sunglasses, which will lessen the harsh light, or you can have the windows on your car tinted, usually the front window and the two side windows of the driver and the front seat passenger.
Every state of the United States has laws and regulations in place to determine how dark the windows of your automobile can be tinted. All sorts of reasons make this is a good policy. But each state realizes that there are medical conditions which allow for these tinted windows to be darker than the rules allow.
Lupus, sunlight allergy, photo-sensitivity and melanoma are some of the medical conditions in which the window tint laws of any state can be waived or altered (a medical exemption) and for the person to avoid a traffic citation. If the car is pulled over, then a driver or passenger must present documentation to the police officer to avoid a traffic ticket being issued. These exemptions are only recognized when they are issued by a medically qualified person who has determined that the driver or passenger qualifies for this exemption by the issuance of a prescription, or detailed letter; this prescription or detailed letter should state the amount of light that is permitted; the prescription must have an expiration date and tell how long the exemption is good for; and the vehicle that is to be used for this medical exemption has to be identified. You can contact the DMV (Department of Motor Vehicles) within your state to determine the exact process you must go through in order to obtain this medical window tinting exemption.
Diabetic retinopathy can affect the ability to see and cause a hypersensitivity to light. If you think that you are in need of one of the special window tinting medical exemptions (medical sun screening), check with your physician to see if you quality and then go through the mandatory steps necessary within your state to qualify. If you qualify for such an exemption, most of the window tinting companies around will know the tint level that is acceptable for your state for a medical condition. Just ask about the services they offer and inquire about their knowledge of the window tinting laws within your state and their knowledge of the medical necessary tinting for those suffering from vision loss of the kind that sunlight worsens. They should have all the rules and regulations right there is their facility. If not, call around until you find a window tinting company that knows all the ins and outs of your state regulations. You don’t want a ticket and run into the expense of having your window tinting removed because it exceeds your state’s requirements so make sure you deal with a qualified, knowledgeable company.
Safety is the most important thing. If your vision is affected by harsh sunlight as a result of your laser surgery to treat your diabetic retinopathy, talk with your ophthalmologist and see if steps can be taken to help you.
 Tom Martinez, Facebook And A Donor: Back in June of 2011, famous quarterback coach Tom Martinez announced on his Facebook page that his
Tom Martinez, Facebook And A Donor: Back in June of 2011, famous quarterback coach Tom Martinez announced on his Facebook page that his 
 New Discoveries Made in Conquering
New Discoveries Made in Conquering  High-Fat Diet
High-Fat Diet  Oil Refining Helping Researchers With New Tools For Type 1 Diabetes: In order to control blood sugar, engineering researchers from the Rensselaer Polytechnic Institute are merging automation techniques from oil refining in order to create a closed-loop
Oil Refining Helping Researchers With New Tools For Type 1 Diabetes: In order to control blood sugar, engineering researchers from the Rensselaer Polytechnic Institute are merging automation techniques from oil refining in order to create a closed-loop  HbA1C Results Prove Inaccurate For Dialysis Patients: According to a new study at Wake Forest Baptist Medical Center, a test known as the golden standard long-term glucose monitoring test proved to be less valuable in patients who are on dialysis.
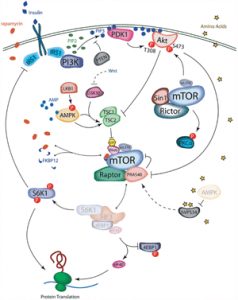
HbA1C Results Prove Inaccurate For Dialysis Patients: According to a new study at Wake Forest Baptist Medical Center, a test known as the golden standard long-term glucose monitoring test proved to be less valuable in patients who are on dialysis. Master Gene Found To Cause Obesity And Diabetes: According to a study led by a team of King’s College London and the University of Oxford researchers, a “master regulator” gene is being named the culprit of high cholesterol levels and type 2 diabetes in the body.
Master Gene Found To Cause Obesity And Diabetes: According to a study led by a team of King’s College London and the University of Oxford researchers, a “master regulator” gene is being named the culprit of high cholesterol levels and type 2 diabetes in the body.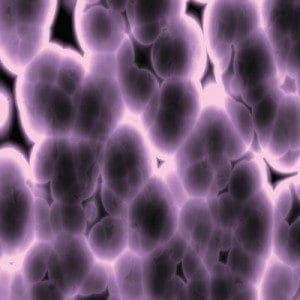 New System Could Convert Cells Into Making
New System Could Convert Cells Into Making 