 Is Tight Blood Sugar Controls Best for Type 2 Diabetes: Should persons with type 2 diabetes keep their blood sugar levels under strict control, resulting in their A1C levels being the same as a person who does not have type 2 diabetes?
Is Tight Blood Sugar Controls Best for Type 2 Diabetes: Should persons with type 2 diabetes keep their blood sugar levels under strict control, resulting in their A1C levels being the same as a person who does not have type 2 diabetes?
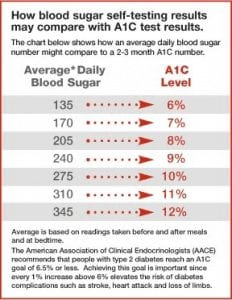
There are known benefits to keeping the blood sugar levels under tight control, but there is also a down side known as “insulin reactions” (hypoglycemia).
A true answer to the benefit of extremely tight control is still unknown.
This is the result of a report that was published by the German Institute for Quality and Efficiency in Health Care (IQWIG) that was recently issued. This compilation report was issued at the request of the Federal Joint Committee (G-BA). IQWIG was requested to prepare the report in a rapid form, meaning no preliminary reports were published. The study involved IQWIG using a randomized controlled trial comparing two treatment strategies in patients with type 2 diabetes. The “test” group measures’ goals were to lower blood sugar levels to near normal levels. In the “control” group measures’ goals there was no attempt to keep blood sugar levels at normal levels. With these two criteria in mind, the goal was to assess the benefit or harm of the interventions for “mortality (all-cause mortality), late complications of diabetes (heart attacks, strokes, damage to the kidneys or eyes, etc.), as well as quality of life.”
IQWIG included seven studies. In those seven studies, 28,000 had participated. Four studies had already been conducted between the 1960s and the 1990s, and the remaining three were after the year 2000. The ethnic origin was specific, Japan, and in some of the studies medications were used that are no longer in use. Rosiglitazone was listed as one such drug.
IQWIG analyzed these studies and their conclusion was that there were no differences between the two groups of “relevant aspects of treatment.” There was no identifiable “advantage or disadvantages found neither for all cause mortality nor for fatal heart attacks, (fatal and non-fatal) strokes, end-stage renal disease (and its pre-stages), amputations, or pre-stages of blindness. Insufficient data were available for the outcomes of quality of life and blindness.”
There were indications that patients with type 2 diabetes did benefit from extremely normal blood sugar levels in the “non-fatal heart attack” area, and it was in this area only. As well, those with the extremely normal blood sugar levels had indications of severe insulin reactions (hypoglycemia) as well as other serious events.
Jurgen Windeler, Director of IQWIG, commented on the current report: “It is quite astonishing: individual interventions, particularly drugs, have in part been well investigated in studies; however, we know relatively little about the advantages and disadvantages of treatment strategies. If doctors are faced with the question as to what they can specifically offer to their diabetes patients, whether they should lower blood glucose levels as much as possible, and in which patients this is a promising (or less promising) approach, they still do not receive satisfactory answers.”
In conclusion, the “few studies available do not allow reliable conclusions.”
 Diagnosing Diabetes and
Diagnosing Diabetes and  Nuts Over Carbs for Diabetes: A recent study shows that when those dealing with type 2 diabetes switched out some of their regular carbohydrates for a half cup of mixed nuts each day, the participants’ blood sugar levels and LDL cholesterol levels dipped slightly over three months. This is no reason to eat nuts all day long, but it’s a good enough reason to think about throwing in some nuts in place of the carbs each day.
Nuts Over Carbs for Diabetes: A recent study shows that when those dealing with type 2 diabetes switched out some of their regular carbohydrates for a half cup of mixed nuts each day, the participants’ blood sugar levels and LDL cholesterol levels dipped slightly over three months. This is no reason to eat nuts all day long, but it’s a good enough reason to think about throwing in some nuts in place of the carbs each day. New Study On Aspirin and Diabetes: A baby aspirin a day can help prevent a heart attack, according to the experts. If you are in the throes of a heart attack, it is recommended that you take a chewable aspirin. We all know there are numerous cases where the use of over-the-counter aspirin can be helpful to the extent that it can save lives.
New Study On Aspirin and Diabetes: A baby aspirin a day can help prevent a heart attack, according to the experts. If you are in the throes of a heart attack, it is recommended that you take a chewable aspirin. We all know there are numerous cases where the use of over-the-counter aspirin can be helpful to the extent that it can save lives. Linagliptin (Tradjenta) Possible Approval for Use in Europe for Type 2 Treatment: Linagliptin (sold under the name Tradjenta) has been available in the United States for those with type 2 diabetes since May 2011, when the Food and Drug Administration gave their approval for its use at that time. Tradjenta is an oral
Linagliptin (Tradjenta) Possible Approval for Use in Europe for Type 2 Treatment: Linagliptin (sold under the name Tradjenta) has been available in the United States for those with type 2 diabetes since May 2011, when the Food and Drug Administration gave their approval for its use at that time. Tradjenta is an oral  Apple Peels, Diabetes and Muscle Wasting: You might not want to peel that apple before eating it, let alone put an apple peel down the garbage disposal or in the trash container under the sink.
Apple Peels, Diabetes and Muscle Wasting: You might not want to peel that apple before eating it, let alone put an apple peel down the garbage disposal or in the trash container under the sink. Zebrafish, Zinc and Diabetes: Zinc is an important trace mineral that people need to stay healthy. Only iron is in stronger form in the body than zinc. Zinc’s highest concentrations are found in the prostate gland and sperm of men, the red and white blood cells, the retinas of the eyes, the liver and the
Zebrafish, Zinc and Diabetes: Zinc is an important trace mineral that people need to stay healthy. Only iron is in stronger form in the body than zinc. Zinc’s highest concentrations are found in the prostate gland and sperm of men, the red and white blood cells, the retinas of the eyes, the liver and the  Study Shows Life Expectancy Longer Now For Type 1 Diabetics:
Study Shows Life Expectancy Longer Now For Type 1 Diabetics:  New Study On Clogged Carotid Arteries And Type 1 Diabetes: Atherosclerosis of the carotid arteries is a buildup of plaque in either the right or left carotid artery, located at the sides on the neck going up to the head. These carotid arteries supply oxygenated blood to the head and neck and are vital for survival. When either of these arteries becomes clogged with plaque, this blood flow to the head and neck can be stopped, and a stroke or a mini-stroke occurs, which could impact a person’s life forever. Usually, the buildup of plaque in the carotid arteries occurs over a period of time.
New Study On Clogged Carotid Arteries And Type 1 Diabetes: Atherosclerosis of the carotid arteries is a buildup of plaque in either the right or left carotid artery, located at the sides on the neck going up to the head. These carotid arteries supply oxygenated blood to the head and neck and are vital for survival. When either of these arteries becomes clogged with plaque, this blood flow to the head and neck can be stopped, and a stroke or a mini-stroke occurs, which could impact a person’s life forever. Usually, the buildup of plaque in the carotid arteries occurs over a period of time. New Drug Delivery Mechanism For
New Drug Delivery Mechanism For