 Glucose Test May Predict Risk of CVD In Diabetes Patients: The most important way to manage ones diabetes is to manage the hemoglobin A1C level within the body. There are many reasons as to why this level is particular is important but one major reason is that by managing it, it can help reduce the risk of cardiovascular disease, also known as CVD.
Glucose Test May Predict Risk of CVD In Diabetes Patients: The most important way to manage ones diabetes is to manage the hemoglobin A1C level within the body. There are many reasons as to why this level is particular is important but one major reason is that by managing it, it can help reduce the risk of cardiovascular disease, also known as CVD.
Through research, diabetes had been noted as a risk factor for cardiovascular disease. However, with patients already suffering from diabetes, the risk is much higher.
Nina P. Paynter, Ph.D., from Brigham and Women’s Hospital, Boston, and colleagues, used data from participants of the Women’s Health Study and the Physician’s Health Study II states, “Simulated cost-benefit analyses have suggested that this variability in CVD risk could provide an opportunity for tailored preventive therapy in diabetic patients.”
Researchers wanted to investigate the importance of HbA 1c levels through a test that reflects the average blood glucose level throughout a period of two months/ three months. Through this test, researchers could see how the HbA 1c affected diabetes and how it was being managed.
Through the test, 24,674 women where used, 685 having diabetes and 11,280 men were used, 563 having diabetes. Through questionnaires, researchers obtained health history and received blood samples to check cholesterol, C-reactive protein and HbA 1c levels. Researchers followed up for a middle point of 10.2 years for women and a midpoint of 11.8 years for men to look for new cases of cardiovascular disease. Their findings consisted of 125 cardiovascular cases in the 685 female surveyors with diabetes and 170 in the 563 male surveyors with diabetes.
The researchers stated, “We found that in these large population-based cohorts of both men and women, presence of diabetes alone did not confer a 10-year risk of CVD higher than 20 percent, and measurement of HbA 1c level in diabetic subjects improved risk prediction compared with classification as cardiovascular risk equivalent. They propose that the difference in risk between the sexes may be partly attributed to the increase in CVD risk with age and the delayed risk in women. Our findings suggest that the improvement in CVD risk prediction, and possibly calibration, obtained with adding HbA 1c levels is highest in lower-risk populations.”
 New Drug Raises HGL Cholesterol And Helps Control Type 2: According to new research, a
New Drug Raises HGL Cholesterol And Helps Control Type 2: According to new research, a  Swamp Gas May Be Used in New Diabetes Treatments: Hydrogen sulfide, more commonly known as “swamp gas” – is responsible for various disagreeable odors, from the smell of rotting plants and sewer systems to certain industrial fumes. Yet a new study supported by the National Institutes of Health, the Juvenile Diabetes Foundation, and Shriners Hospital for Children and conducted by the University of Texas Medical Branch at Galveston suggests that this foul-smelling compound plays an important role in shielding blood vessels from the effects of diabetes.
Swamp Gas May Be Used in New Diabetes Treatments: Hydrogen sulfide, more commonly known as “swamp gas” – is responsible for various disagreeable odors, from the smell of rotting plants and sewer systems to certain industrial fumes. Yet a new study supported by the National Institutes of Health, the Juvenile Diabetes Foundation, and Shriners Hospital for Children and conducted by the University of Texas Medical Branch at Galveston suggests that this foul-smelling compound plays an important role in shielding blood vessels from the effects of diabetes. Body Muscle Mass Helps Fight
Body Muscle Mass Helps Fight  Cell Phones Helping Manage Diabetes: According to a new study from the University Of Maryland School Of Medicine, an interactive computer software program could be very effective in helping patients with type 2 diabetes, manage their diabetes using their mobile phone.
Cell Phones Helping Manage Diabetes: According to a new study from the University Of Maryland School Of Medicine, an interactive computer software program could be very effective in helping patients with type 2 diabetes, manage their diabetes using their mobile phone. New Research – Stem Cell Memory and
New Research – Stem Cell Memory and  No Higher Risk for Type 2 Diabetes In Natural Menopause versus Ovarian Removal Menopause: Whether menopause comes naturally as a female ages or is brought on at an earlier age due to a hysterectomy that involves ovary removal, there is no increase in the diagnosis of type 2 diabetes, and the risk for type 2 diabetes does not increase.
No Higher Risk for Type 2 Diabetes In Natural Menopause versus Ovarian Removal Menopause: Whether menopause comes naturally as a female ages or is brought on at an earlier age due to a hysterectomy that involves ovary removal, there is no increase in the diagnosis of type 2 diabetes, and the risk for type 2 diabetes does not increase.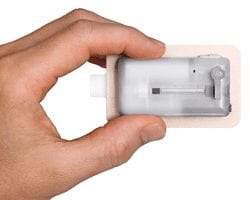 V-Go Disposable
V-Go Disposable 
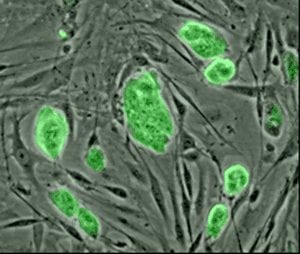 Diabetes Cure:
Diabetes Cure: