 New research shows that neither intake of vitamin D nor circulating levels of 25(OH)D are associated with increased risk of islet autoimmunity (IA) or the development of Type 1 diabetes in young children. The findings appear to be at odds with earlier research, which contradicted the conclusions of the study. The study was published in the journal Diabetologia.
New research shows that neither intake of vitamin D nor circulating levels of 25(OH)D are associated with increased risk of islet autoimmunity (IA) or the development of Type 1 diabetes in young children. The findings appear to be at odds with earlier research, which contradicted the conclusions of the study. The study was published in the journal Diabetologia.
The study involved 198 children who had developed islet autoimmunity among an original group of 2,644 children in the U.S. Researchers regularly measured both vitamin D intake and 25(OH)D levels in the children. 128 of the children had been diagnosed with plasma 25(OH)D levels in a check-up at nine months of age.
Neither vitamin D intake nor 25(OH)D levels were shown to be associated with an increased risk of islet autoimmunity, even after adjusting for confounding factors such as Type 1 diabetes, DQB1*0302 genotype, ethnicity, and HLA-DR3/4.
Researchers measured the antibodies present in the children at the ages of nine, 15, and 24 months. They measured vitamin D intake through parent questionnaires that inquired about the frequency of eating certain foods until the children were nine years old; at 10, the researchers obtained the information from the children directly.
The research team acknowledged that the findings of the study were “somewhat contradictory” to previous research on the subject, which suggested that supplementing the diet of infants with vitamin D could offer a protective effect against Type 1 diabetes.
“Our study, which uses a powerful combination of prospectively collected reports of vitamin D intake and a biomarker of vitamin D status, does not support an association between a child’s usual vitamin D intake or 25(OH)D levels… and the risk of IA (islet autoimmunity) or progression to type I diabetes,” said the research team.
They noted that they still needed to test the actual effects of vitamin D supplements during infancy — whether low intake of vitamin D was harmful or very high intake was beneficial.
Earlier this year, Anastassios Pittas, M.D., with Tufts Medical Center in Boston, presented research findings at the annual meeting of the American Diabetes Association suggesting that higher levels of vitamin D in the blood were associated with a reduced risk of developing Type 2 diabetes. However, the study does not prove a cause-effect relationship, simply a correlation. Though the findings are not enough to provide a direct causal relationship, Dr. Pittas stated that if the findings were confirmed, “…there are huge implications because vitamin D is easy and inexpensive.”
Similarly, a study presented in 2010 at the annual meeting of the Endocrine Society by Dr. Esther Krug, M.D., appeared to show that vitamin D deficiency could be a risk factor for glucose intolerance and that such deficiencies are commonly noted in people with poor diabetes control. Again, the study did not prove a cause and effect relationship between vitamin D levels and diabetes, but it suggested a correlation. As vitamin D deficiencies became more pronounced in the study participants, their diabetes control worsened.
Vitamin D is naturally present in very few foods. Some foods are fortified with vitamin D while many people take dietary supplements. It is also produced when sunlight hits the skin, which begins the vitamin D synthesis process. Vitamin D is important for calcium absorption; it is necessary for bone growth and bone remodeling, and without the vitamin, bones can become weak and brittle. Vitamin D thus helps older adults prevent osteoporosis in addition to its many roles throughout the body.
 Amelia Lily, the 16-year-old Lady Gaga fan who performs on the British television talent show X-Factor, seems bound for stardom. She recently gave a performance of Janis Joplin’s Piece of My Heart which had one judge saying, “That was amazing. You blew up the stage.” The judge added, “People work their whole lives and take forever to get to the level that you are at now, you’ve come on that stage so much older than your years.” X Factor is a singing talent show created by Simon Cowell, who also created American Idol.
Amelia Lily, the 16-year-old Lady Gaga fan who performs on the British television talent show X-Factor, seems bound for stardom. She recently gave a performance of Janis Joplin’s Piece of My Heart which had one judge saying, “That was amazing. You blew up the stage.” The judge added, “People work their whole lives and take forever to get to the level that you are at now, you’ve come on that stage so much older than your years.” X Factor is a singing talent show created by Simon Cowell, who also created American Idol. Sensors for Medicine and Science announced that its implanted continuous glucose sensor, which the company is currently developing, has demonstrated highly accurate results. The sensor tracked glucose levels in study participants with a 77.6% accuracy in the A zone of the Clark Error Grid and a 19.2% in the B zone of the grid, resulting in a mean absolute difference of 12.2%. It is the first time an implant-based sensor has achieved such accuracy. The study also achieved the goal of continuous sensor use in patients for over six months.
Sensors for Medicine and Science announced that its implanted continuous glucose sensor, which the company is currently developing, has demonstrated highly accurate results. The sensor tracked glucose levels in study participants with a 77.6% accuracy in the A zone of the Clark Error Grid and a 19.2% in the B zone of the grid, resulting in a mean absolute difference of 12.2%. It is the first time an implant-based sensor has achieved such accuracy. The study also achieved the goal of continuous sensor use in patients for over six months. Researchers in Jerusalem have identified a possible cure for Type 1 diabetes in the form of a signal that activates regeneration of pancreatic beta cells, which are responsible for producing
Researchers in Jerusalem have identified a possible cure for Type 1 diabetes in the form of a signal that activates regeneration of pancreatic beta cells, which are responsible for producing 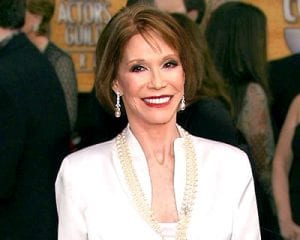 The Screen Actors Guild is awarding Mary Tyler Moore, known for her roles in 60s and 70s television with “The Dick Van Dyke Show” and “The Mary Tyler Moore Show” as well as her work in promoting diabetes research, with the lifetime achievement award.
The Screen Actors Guild is awarding Mary Tyler Moore, known for her roles in 60s and 70s television with “The Dick Van Dyke Show” and “The Mary Tyler Moore Show” as well as her work in promoting diabetes research, with the lifetime achievement award.
 Today, almost 26 million Americans — adults and children — have been diagnosed with diabetes. By 2025, that number is projected to rise to 438 million individuals around the world, which would be about 7.8% of the world’s adult population. Combating the rise of diabetes involves multifaceted strategies but promoting a healthy diet is one of the most effective ways of reducing the numbers of the disease. Two recent studies have shown that a common food source can aid in the fight against diabetes, suggesting that including almonds in the diet of a Type 2 diabetic can help to regulate blood sugar and cholesterol levels.
Today, almost 26 million Americans — adults and children — have been diagnosed with diabetes. By 2025, that number is projected to rise to 438 million individuals around the world, which would be about 7.8% of the world’s adult population. Combating the rise of diabetes involves multifaceted strategies but promoting a healthy diet is one of the most effective ways of reducing the numbers of the disease. Two recent studies have shown that a common food source can aid in the fight against diabetes, suggesting that including almonds in the diet of a Type 2 diabetic can help to regulate blood sugar and cholesterol levels. A study that analyzed over 3,400 French adults over a period of 14 years found that those with Type 2 diabetes who received
A study that analyzed over 3,400 French adults over a period of 14 years found that those with Type 2 diabetes who received 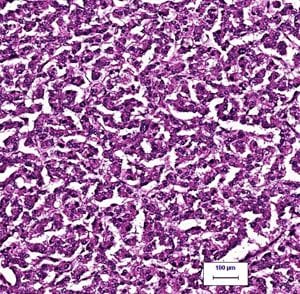 For decades, scientists have been trying to identify the molecules that activate beta cell growth in the fight against diabetes. Once these molecules are identified, scientists could develop therapeutics that target them. One research team, funded by the Juvenile Diabetes Research Fund in collaboration with pharmaceutical manufacturer Hoffman-La Roche, recently made significant headway in this area of diabetes research by discovering a
For decades, scientists have been trying to identify the molecules that activate beta cell growth in the fight against diabetes. Once these molecules are identified, scientists could develop therapeutics that target them. One research team, funded by the Juvenile Diabetes Research Fund in collaboration with pharmaceutical manufacturer Hoffman-La Roche, recently made significant headway in this area of diabetes research by discovering a  A joint study conducted by the Scripps Research Institute and the Dana-Farber Cancer Institute at Harvard University has discovered a new type of anti-diabetic therapeutic that works by targeting a particular molecular switch.
A joint study conducted by the Scripps Research Institute and the Dana-Farber Cancer Institute at Harvard University has discovered a new type of anti-diabetic therapeutic that works by targeting a particular molecular switch.