 Patients who have been diagnosed with Type 2 diabetes can demonstrate elevated levels of glucose and glycated hemoglobin (HbA1c) even 10 years before their actual diagnosis, according to Esther van’t Riet, Ph.D., with the Department of Epidemiology and Biostatistics at VU University Medical Center in Amsterdam. Dr. van’t Riet presented the information at a poster session at the 47th annual meeting of the European Association for the Study of Diabetes (EASD). According to Dr. van’t Riet, individuals demonstrate moderate increases and then rapid increases in the few years prior to the diagnosis of diabetes, with increases in Hba1c often preceding elevated glucose.
Patients who have been diagnosed with Type 2 diabetes can demonstrate elevated levels of glucose and glycated hemoglobin (HbA1c) even 10 years before their actual diagnosis, according to Esther van’t Riet, Ph.D., with the Department of Epidemiology and Biostatistics at VU University Medical Center in Amsterdam. Dr. van’t Riet presented the information at a poster session at the 47th annual meeting of the European Association for the Study of Diabetes (EASD). According to Dr. van’t Riet, individuals demonstrate moderate increases and then rapid increases in the few years prior to the diagnosis of diabetes, with increases in Hba1c often preceding elevated glucose.
Dr. van’t Riet and her research team used data from the Hoorn Study, a cohort of 565 Dutch participants, aged 50 to 75 at baseline in 1989 and with follow-ups in 1996 and 2000. None of the 565 participants had been diagnosed with diabetes at the beginning of the study.
At follow-up meetings, incident diabetes was diagnosed with the World Health Organization and American Diabetes Association’s 2011 criteria for the disease: fasting blood glucose levels of 7.0 mmol/L (126.1 mg/dL) or greater, or post-load glucose levels of 11.1 mmol/L (200mg/dL) or higher; and/or HbA1c levels of 6.5% or higher. Participants were categorized according to the status of their development of diabetes at baseline and follow-up.
At the 1996 follow-up, 99 of the study participants had developed incident diabetes; by 2000, an additional 48 had developed the disease. At the 2000 follow-up, 418 participants had still not developed diabetes. According to van’t Riet, the development of diabetes was preceded by elevated glucose and HbA1c levels in the years leading up to the diagnosis. “Those who developed diabetes already had elevated levels of glucose and A1c in 1989. So up to 10 years before diagnosis, we already see an elevation of all 3 glycemic measures,” she said. The third measure that the study analyzed was post-load glucose levels, which were obtained two hours into an oral glucose tolerance test.
“When we look at changes in time, we first compared those who never developed diabetes with those who had insulin diabetes in 1996. We see that all 3 glycemic measures show a steep increase from 1989 to 1996. After the diagnosis in 1996, they stabilize,” said Dr. van’t Riet.
The researchers also compared study participants who didn’t develop diabetes throughout the course of the investigation with those who had developed the disease in 2000. Those who developed diabetes saw increases in fasting glucose and post-load glucose between 1989 and 1996 that was “almost comparable for those who developed diabetes and those who never developed diabetes.” However, by 1996, those levels increased in the group that developed diabetes: “A steep increase is observed, which was not seen in those who never developed diabetes,” said dr. van’t Riet.
Unlike blood glucose levels, HbA1c levels did increase between 1989 and 1996 for those who later developed diabetes. “This might indicate that A1c increases earlier than glucose,” said Dr. van’t Riet.
The researchers performed further analysis on study participants with incident diabetes in 2000 who had increased HbA1c levels but lower glucose, and on those who had high glucose and normal HbA1c due to changes in the diagnostic criteria for diabetes.
“In those with diabetes based on high glucose, A1c levels tend to increase also. But in those with diabetes based on high A1c, glucose levels tend to stabilize in the follow-up period…. It might indicate that there are different developmental patterns according to the type of criteria you use,” continued van’t Riet.
 Doctors have long extolled the health values of getting eight hours of sleep every night. Add another benefit to the list: new research shows that getting eight and a half hours of sleep every night could reduce the risk of developing Type 2 diabetes in teenagers who are obese. The findings were published in the journal “Diabetes Care.”
Doctors have long extolled the health values of getting eight hours of sleep every night. Add another benefit to the list: new research shows that getting eight and a half hours of sleep every night could reduce the risk of developing Type 2 diabetes in teenagers who are obese. The findings were published in the journal “Diabetes Care.”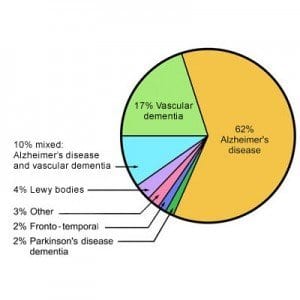 A longitudinal study conducted in Japan has shown that risk of dementia increases when glucose levels swing out of control, especially directly after
A longitudinal study conducted in Japan has shown that risk of dementia increases when glucose levels swing out of control, especially directly after 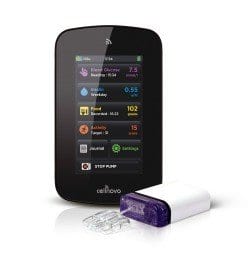 Cellnovo, a company working towards the development of new
Cellnovo, a company working towards the development of new 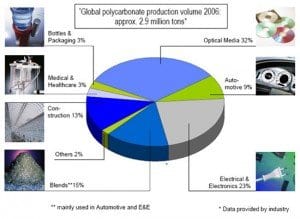 A recent study of 3,400 Chinese adults, age 40 and over, has found that exposure to bisphenol A is not associated with an increased risk of developing diabetes. Bisphenol A is a chemical used in plastics that has been surrounded by controversy since some claimed it was responsible for health problems. The findings were published in the journal “Annals of Internal Medicine.”
A recent study of 3,400 Chinese adults, age 40 and over, has found that exposure to bisphenol A is not associated with an increased risk of developing diabetes. Bisphenol A is a chemical used in plastics that has been surrounded by controversy since some claimed it was responsible for health problems. The findings were published in the journal “Annals of Internal Medicine.” A study conducted on elderly (over 65) patients who had been diagnosed with Type 2 diabetes found that they were not as aware of their own hypoglycemic conditions as were middle-aged (age 39-64) patients.
A study conducted on elderly (over 65) patients who had been diagnosed with Type 2 diabetes found that they were not as aware of their own hypoglycemic conditions as were middle-aged (age 39-64) patients. Mutinational pharmaceutical company Novartis recently announced at the 47th annual Meeting of the European Association for the Study of Diabetes that results from a recent study demonstrated that Galvus® (vidagliptin) is similar in safety profile to placebo when it is used in conjunction with other anti-diabetic therapies in patients who have Type 2 diabetes and moderate to several renal impairment. The study, sponsored by Novartis, also showed that vidagliptin significantly improved glycemic control when it was added to current therapies.
Mutinational pharmaceutical company Novartis recently announced at the 47th annual Meeting of the European Association for the Study of Diabetes that results from a recent study demonstrated that Galvus® (vidagliptin) is similar in safety profile to placebo when it is used in conjunction with other anti-diabetic therapies in patients who have Type 2 diabetes and moderate to several renal impairment. The study, sponsored by Novartis, also showed that vidagliptin significantly improved glycemic control when it was added to current therapies. A Phase III investigation of linagliptin (trade name Trajenta® in Europe) that lasted 102 weeks has shown significantly lowered blood glucose levels in adults who have been diagnosed with Type 2 diabetes. The results of the study were presented at the 47th yearly meeting of the European Association for the Study of Diabetes (EASD) by Boehringer Ingelheim and Eli Lilly and Company. The findings demonstrated that linagliptin, a DPP-4 inhibitor, showed a positive safety profile in addition to reducing HbA1c levels by 0.8% over a long term period in patients who were treated with the
A Phase III investigation of linagliptin (trade name Trajenta® in Europe) that lasted 102 weeks has shown significantly lowered blood glucose levels in adults who have been diagnosed with Type 2 diabetes. The results of the study were presented at the 47th yearly meeting of the European Association for the Study of Diabetes (EASD) by Boehringer Ingelheim and Eli Lilly and Company. The findings demonstrated that linagliptin, a DPP-4 inhibitor, showed a positive safety profile in addition to reducing HbA1c levels by 0.8% over a long term period in patients who were treated with the 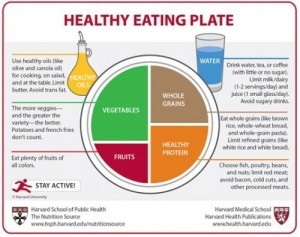 The U.S. Department of Agriculture has long held the food pyramid in high esteem as a recommendation for the types of foods we should be eating and their ratios to other foods. Within recent months, however, the USDA has redesigned its nutritional recommendations in the form of a plate, with portions of
The U.S. Department of Agriculture has long held the food pyramid in high esteem as a recommendation for the types of foods we should be eating and their ratios to other foods. Within recent months, however, the USDA has redesigned its nutritional recommendations in the form of a plate, with portions of 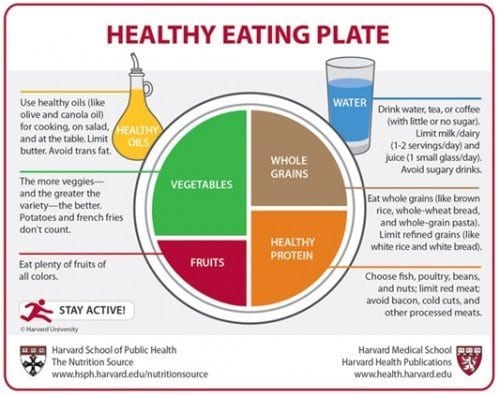
 A registry analysis reports that patients who had been diagnosed with Type 2 diabetes and used
A registry analysis reports that patients who had been diagnosed with Type 2 diabetes and used