 According to researchers at the University of Cambridge in the United Kingdom, a rare and serious form of hypoglycemia can be traced back to a hereditary disposition.
According to researchers at the University of Cambridge in the United Kingdom, a rare and serious form of hypoglycemia can be traced back to a hereditary disposition.
The scientists say that the AKT2 gene — or more specifically, mutations in the gene — are responsible for causing this particular type of hypoglycemia, which is serious enough to be considered life-threatening and which deprives the body of the energy it needs to continue functioning normally.
According to the scientists from Cambridge, who published their report in the journal “Science,” there are already cancer drugs in use which are designed to treat a similar process.
Hypoglycemia, or a condition of low blood sugar, can be caused by imbalances between blood sugar levels and insulin, which carries sugar away from the bloodstream and into cells, lowering blood glucose levels. Hypoglycemia typically occurs in individuals who have Type 1 diabetes, when they miss meals, consume alcohol, or inject themselves with too much insulin.
The researchers at the University of Cambridge discovered that one in 100,000 babies is born with a mutation in the AKT2 gene that causes hypoglycemic conditions even when no insulin is present in the blood. In those cases, individuals should exhibit high levels of blood glucose.
Individuals with this mutation must use feeding tubes during periods of sleep to ensure that blood sugar levels do not drop too low. The patient must always be vigilant about maintaining blood sugar levels and ensuring that they don’t dip into dangerous territory, and the condition can be taxing for both the patient and his or her family.
“Fear of low blood sugar has dominated the lives of these patients and their families,” said Dr. Robert Semple, one of the researchers from Cambridge.
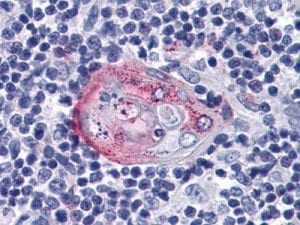
In discovering the mutation, the scientists looked at genetic code of three children who had this severe form of hypoglycemia. All of the children exhibited a certain mutation in the ATK2 gene. The mutation causes the ATK2 gene, which functions as an interpreter for insulin, to act as if insulin is always being produced by the pancreas. Blood sugar levels are therefore consistently lowered.
According to Professor Stephen O’Rahilly, lead researcher on the project at Cambridge, there are medications available which target ATK1 and also provide some effect in acting on ATK2. These medications are currently used to treat cancer. Since medications already exist which act on the genes, it may not be long before new treatments are introduced for treating the rare form of hypoglycemia.
“There are actual pills that can be swallowed by humans. There could be a treatment in a year,” said Professor O’Rahilly.
An individual is considered hypoglycemic when his or her blood sugar levels fall below 70mg/dL. If blood sugar levels remain at such a low level for an extended period of time, it can be harmful to the individual. The hormone insulin is normally produced by the beta cells of the pancreas where it works to reduce blood sugar levels, but blood sugar levels can fall too low if too much insulin is produced, exercise is performed at a different time, or alcohol is consumed, among other factors. Hypoglycemia is treated by consuming about 15 grams of carbohydrates and checking blood sugar levels again after about 15 minutes. Hypoglycemia can cause loss of consciousness and even seizures or nervous system damage; as such, it should be treated as quickly as possible, but individuals with low blood sugar should refrain from driving themselves to reach a hospital.
 Juvisync, a pill that combines
Juvisync, a pill that combines  A study conducted at the University of Wisconsin-Madison has identified a gene that could increase susceptibility to diabetes in those who carry it. Researchers discovered the gene in obese mice; it controls a
A study conducted at the University of Wisconsin-Madison has identified a gene that could increase susceptibility to diabetes in those who carry it. Researchers discovered the gene in obese mice; it controls a 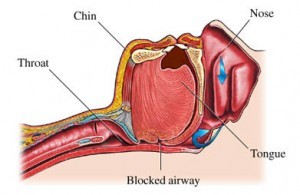 An ancillary study to the Look AHEAD trial found that intensive lifestyle interventions designed to promote weight loss in obese individuals with Type 2 diabetes also helped reduce obstructive
An ancillary study to the Look AHEAD trial found that intensive lifestyle interventions designed to promote weight loss in obese individuals with Type 2 diabetes also helped reduce obstructive  New research has demonstrated that a type of sugar extracted from buckwheat, called D-fagomine, could help diabetics keep their blood glucose levels well-managed and may offer prebiotic activity in small doses.
New research has demonstrated that a type of sugar extracted from buckwheat, called D-fagomine, could help diabetics keep their blood glucose levels well-managed and may offer prebiotic activity in small doses.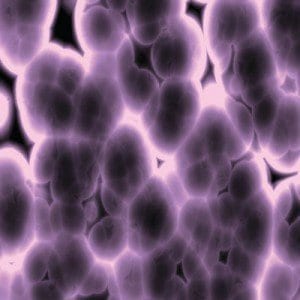 A team of scientists reported on October 5 that they had successfully utilized cloning technology to create
A team of scientists reported on October 5 that they had successfully utilized cloning technology to create 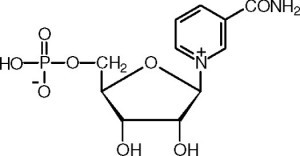 A team of United States-based scientists are hopeful that new research on a natural chemical found in body cells could set the stage for the development of a vitamin-like pill that could prevent diabetes or perhaps even reverse the disease completely.
A team of United States-based scientists are hopeful that new research on a natural chemical found in body cells could set the stage for the development of a vitamin-like pill that could prevent diabetes or perhaps even reverse the disease completely. A study published in the October issue of the journal “Diabetes Care” has demonstrated that, in patients with Type 1 diabetes who receive intensive
A study published in the October issue of the journal “Diabetes Care” has demonstrated that, in patients with Type 1 diabetes who receive intensive  A recent randomized trial showed that increasing the intensity of weight loss interventions only in patients who do not succeed in reaching their goals may be an effective alternative to typical approaches.
A recent randomized trial showed that increasing the intensity of weight loss interventions only in patients who do not succeed in reaching their goals may be an effective alternative to typical approaches. A new study warns that eating food too quickly more than doubles an individual’s chance of developing impaired glucose tolerance, also known as
A new study warns that eating food too quickly more than doubles an individual’s chance of developing impaired glucose tolerance, also known as