 The latest statistics of the International Diabetes Federation predict that diabetes rates will continue to rise in the coming years. By 2030, the IDF predicts, 552 million people could have the disease, or at least one in 10 adults worldwide.
The latest statistics of the International Diabetes Federation predict that diabetes rates will continue to rise in the coming years. By 2030, the IDF predicts, 552 million people could have the disease, or at least one in 10 adults worldwide.
The November 14 report from the IDF used factors such as demographic changes and aging to predict the increasing rates of the disease. According to the IDF, about one in 13 adults worldwide now has diabetes.
The number includes both variants of diabetes in addition to undiagnosed cases. The IDF predicts that the number of diabetes cases will jump significantly—about 90 percent—in Africa, where infectious diseases have typically claimed more lives than diabetes. The predictions may even be conservative, since increasing rates of diabetes due to obesity were not taken into account.
Today, the World Health Organization estimates that there are 346 million people living with diabetes around the world; over 80 percent of deaths from diabetes occur in developing countries. The WHO predicts that diabetes deaths will double by the year 2030 and that the International Diabetes Federation’s numbers are possible.
According to Gojka Roglic, the head of the diabetes unit at the WHO, the predictions are “a credible figure.”
“But whether or not it’s correct, we can’t say,” continued Roglic. She noted that the increasing rates of obesity were linked to the aging of the population rather than the obesity epidemic, although most people with diabetes have the Type 2 variant of the disease, which is related to obesity, poor diet and lack of exercise.
The good news is that many cases of Type 2 diabetes are preventable. “It’s worrying because these people will have an illness which is serious, debilitating, and shortens their lives,” said Roglic. “But it doesn’t have to happen if we take the right interventions.”
Such interventions could include counseling on healthy eating and getting regular exercise. Research has demonstrated that interventions which improve or reverse obesity and sedentary lifestyles are also helpful in controlling blood glucose levels in diabetes. In patients who receive both bariatric surgery and interventions to reduce risk factors of diabetes, the disease is almost completely eliminated.
The number of Type 2 diabetes cases has grown by leaps and bounds over the past several decades. In 1985, the IDF estimated that about 30 million people around the world had diabetes. By 2000, that number had increased to 150 million, and today estimates place the number around 366 million people. Half of those with diabetes are between the ages of 20 and 60, and the disease is expected to grow exponentially. About 4.6 million people die from diabetes each year; the disease also takes an immense financial toll due to health care costs, which run about $465 billion each year in treatment for the disease.
“The data from the latest edition of the IDF Diabetes Atlas show that the epidemic is out of control,” said Professor Jean Claude Mbanya, President of the IDF. “We are losing ground in the struggle to contain diabetes. No country is immune and no country is fully equipped to repel this common enemy.”
The International Diabetes Federation is an association of over 200 diabetes organizations, spanning over 160 countries around the world. Since 1950, the IDF has promoted awareness of the disease, proper care and prevention, and the search for a cure for both Type 1 and Type 2 diabetes.
 Diabetics around the world are familiar with the routine of blood glucose testing that requires a prick on the finger to draw blood. Though the inconvenience of drawing blood is a small price to pay for accurate blood sugar control, some diabetics require several tests a day and the frequent pricks can be tiring.
Diabetics around the world are familiar with the routine of blood glucose testing that requires a prick on the finger to draw blood. Though the inconvenience of drawing blood is a small price to pay for accurate blood sugar control, some diabetics require several tests a day and the frequent pricks can be tiring. Medtronic, Inc., the world’s largest medical technology company, recently announced that it received approval from the U.S. Food and Drug Administration for its Investigational Device Exemption (IDE) in conducting a pivotal clinical trial in the ASPIRE study, an investigation of the in-home efficacy of the Low Glucose Suspend feature of Medtronic’s MiniMed Paradigm
Medtronic, Inc., the world’s largest medical technology company, recently announced that it received approval from the U.S. Food and Drug Administration for its Investigational Device Exemption (IDE) in conducting a pivotal clinical trial in the ASPIRE study, an investigation of the in-home efficacy of the Low Glucose Suspend feature of Medtronic’s MiniMed Paradigm  Findings from a new study suggest that people who have previously suffered from
Findings from a new study suggest that people who have previously suffered from  A new study suggests that doctors may be able to help diagnose diabetes and related warning signs through the use of a “muffin test.” The test would be a type of oral glucose tolerance test designed to identify diabetes and impaired glucose tolerance by analyzing the body’s ability to utilize glucose properly.
A new study suggests that doctors may be able to help diagnose diabetes and related warning signs through the use of a “muffin test.” The test would be a type of oral glucose tolerance test designed to identify diabetes and impaired glucose tolerance by analyzing the body’s ability to utilize glucose properly. Two former graduate students at MIT’s George R. Harrison Spectroscopy Laboratory have developed new spectrograph technology that could allow diabetics to monitor their blood glucose levels without pricking their fingers to draw blood for testing. Kong and Barman significantly reduced the size of the spectrograph, allowing the technology to be used in much more convenient spaces.
Two former graduate students at MIT’s George R. Harrison Spectroscopy Laboratory have developed new spectrograph technology that could allow diabetics to monitor their blood glucose levels without pricking their fingers to draw blood for testing. Kong and Barman significantly reduced the size of the spectrograph, allowing the technology to be used in much more convenient spaces. Researchers located in the United Kingdom say that levels of a hormone called B-type natriuretic peptide could have a role in reducing risk of Type 2 diabetes. The study was published online in the journal “PLoS Medicine.”
Researchers located in the United Kingdom say that levels of a hormone called B-type natriuretic peptide could have a role in reducing risk of Type 2 diabetes. The study was published online in the journal “PLoS Medicine.” The American Diabetes Association recently released a position statement which stated that, in helping young people transition into more responsible roles for managing their own diabetes, parents should gradually transfer the responsibilities associated with the disease to their children.
The American Diabetes Association recently released a position statement which stated that, in helping young people transition into more responsible roles for managing their own diabetes, parents should gradually transfer the responsibilities associated with the disease to their children.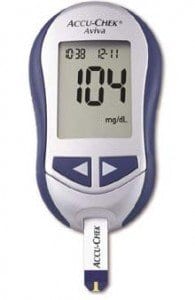 A recent investigation found that U.S. adults who have been diagnosed with diabetes are about two times more likely to contract hepatitis B infections. The findings prompted a recommendation to the Centers for Disease Control and
A recent investigation found that U.S. adults who have been diagnosed with diabetes are about two times more likely to contract hepatitis B infections. The findings prompted a recommendation to the Centers for Disease Control and  New research suggests that drinking less than a couple of glasses of water every day increases an individual’s risk of having elevated blood sugar levels in an unhealthy range.
New research suggests that drinking less than a couple of glasses of water every day increases an individual’s risk of having elevated blood sugar levels in an unhealthy range.