 MircoRNAS: Increased Risk of Amputations: Diabetes is more common in today’s society than it was years ago. More than 24 million people have been diagnosed with diabetes, while there are millions of others who have it, yet have not been diagnosed and another million people will be diagnosed, just this year. Through research and major advances in medical science, there have been some really great strides in trying to find a cure. However, through a new study, researchers have found a cause for the need of so many amputations.
MircoRNAS: Increased Risk of Amputations: Diabetes is more common in today’s society than it was years ago. More than 24 million people have been diagnosed with diabetes, while there are millions of others who have it, yet have not been diagnosed and another million people will be diagnosed, just this year. Through research and major advances in medical science, there have been some really great strides in trying to find a cure. However, through a new study, researchers have found a cause for the need of so many amputations.
A person who has diabetes throughout most of their life, could have an amputation, mainly due to an ulcer that will not heal, due to the lack of blood flow to a general area. Through new studies, researchers have found that one of the diminutive entities within the human genome called Mirco-RNA’s could be the contributing factor to limb amputation in diabetic patients who have poor circulation.
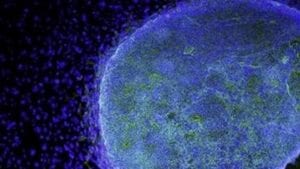
This study was completed by Dr. Andrea Caporali and other colleagues in Professor Costanza Emanueli’s research group in the Regenerative Medicine Section of the School of Clinical Sciences at the University of Bristol. This study was funded by the Medical Research Council. The researchers showed an experimental cell study in which conditions the mocking of diabetes and a lack of blood supply to a tissue increased specific miRNA called, MiRNA-503 and also impaired that ability of endothelial cells. Endothelial cells line the inner shell of a blood vessel. Mirco-RNAS are diminutive sectors of ribonucleic acid (RNA) that can obstruct numerous genes. Through this study, researchers tried slowing the miRNA-503, which helped to increase the ability of endothelial cells. They began to replicate and form into systems of small blood vessels. Through the study of miRNA-503, researchers established that cell growth was decreased and a prevention of configuration of blood cells by straight binding and an inhibition of cyclin E1 and Cdc25 mRNA.
Here is what Constanza Emanueli stated about the research, “Because each miRNA can regulate many genes, they represent an exciting new target to correct diseases that have complex underlying mechanisms, like diabetes, rather than trying to target one specific gene. Our study is the first to provide evidence for a role of miRNAs in diabetes-induced defects in reparative angiogenesis.”
For the study, a team investigated miRNA-503 and targeted gene expression in muscular specimens from the amputated ischaemic legs of diabetic patients. Severed calf biopsies of non-diabetic and non-ischemic patients enduring vein shredding were used. Researchers noticed that miR-503 illustration had increased, and plasma miR-503 levels were also increased as well. Through the use of mouse models that have diabetes and limb ischaemia, researchers found the inhibition of the miRNA-503 by using a decoy miRNA could help restore post-ischaemic blood flow mending.
Individuals diagnosed with diabetes face the hardship of damaged blood vessels via high blood glucose levels, early on. This leads to lack of blood flow (ischaemia) and causes many complications down the road such as disease and even sometimes, death in individuals with diabetes. Usually, an ulcer will appear on a diabetic limb, usually one that will not heal, it is followed by the ischaemic disease, which starts a domino effect. Typically, the only way to provide treatment and healing is use limb amputation. With this new found study, maybe there is new hope for those suffering from lack of blood flow. Perhaps, a new treatment can be provided and amputations will become a thing of the past.
 New Study Shows Coffee Protects Against Diabetes: Coffee is a great way to wake up in the morning. In fact, millions of people surveyed say, that they are not themselves until they have at least had one cup of Joe in the morning. It is the jump-start many people need in the morning, but researchers find that it is having quite a different effect, on personal health.
New Study Shows Coffee Protects Against Diabetes: Coffee is a great way to wake up in the morning. In fact, millions of people surveyed say, that they are not themselves until they have at least had one cup of Joe in the morning. It is the jump-start many people need in the morning, but researchers find that it is having quite a different effect, on personal health. PhysioLab® Platform and Biomarkers: Researchers at the La Jolla Institute have discovered how to use a computer model to mark the biomarkers in the onset of type 1 diabetes.
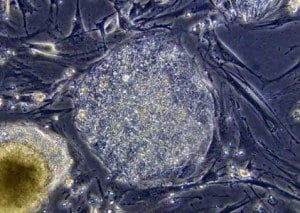
PhysioLab® Platform and Biomarkers: Researchers at the La Jolla Institute have discovered how to use a computer model to mark the biomarkers in the onset of type 1 diabetes.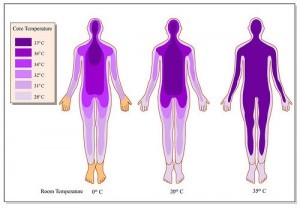 Body Temperature and
Body Temperature and 

 Can Cell Switching Help Diabetes: Diabetes is a very tough health issue that millions of people around the world deal with every single day. Those who have diabetes know how disconcerting it is to have to stop mid-day and do a blood test. Diabetes takes a lot out of a person and when it is not treated; there are so many wrong things that can happen in the future from toe
Can Cell Switching Help Diabetes: Diabetes is a very tough health issue that millions of people around the world deal with every single day. Those who have diabetes know how disconcerting it is to have to stop mid-day and do a blood test. Diabetes takes a lot out of a person and when it is not treated; there are so many wrong things that can happen in the future from toe