Oil Refining Helping Researchers With New Tools For Type 1 Diabetes: In order to control blood sugar, engineering researchers from the Rensselaer Polytechnic Institute are merging automation techniques from oil refining in order to create a closed-loop artificial pancreas.
Oil Refining Helping Researchers With New Tools For Type 1 Diabetes: In order to control blood sugar, engineering researchers from the Rensselaer Polytechnic Institute are merging automation techniques from oil refining in order to create a closed-loop artificial pancreas.
The reason for this device is so that blood sugar levels can be automatically monitored and insulin can be administered to patients suffering from Type 1 diabetes. After six years of research and studies, Professor B. Wayne Bequette, a member of the Department of Chemical and Biological Engineering at Rensselaer had progressively created more highly advanced control systems for the closed-loop artificial pancreas. Through Professor Bequette work, he hopes to benefit 15,000 children and 15,000 adults who are diagnosed with Type 1 diabetes every single year.
Bequette states: “Every single person with Type 1 diabetes has a different response to insulin and a different response to meals. These responses also vary with the time of day, type of meal, stress level, and exercise. A successful automated system must be safe and reliable in spite of these widely varying responses.”
Like most people, Bequettes fight against type 1 diabetes is very personal to him, given that his little sister developed the disease very early in life. Unfortunately, at that time diabetes wellness was not as advanced as it is today.
A person who had Type 1 diabetes will find themselves with little or no insulin in their pancreas. Due to this, they will have to take insulin injections on a daily basis. Some people who have Type 1 diabetes prefer to use an insulin pump instead. The insulin will help to maintain the blood sugars, for if they do not stay balanced serious life-threatening health problems could occur through hyperglycemic, which means blood sugar is too high and through hypoglycemic, which means blood sugar is too low.
Bequette says, “A key challenge for people living with Type 1 diabetes is the constant monitoring of their blood sugar level. Blood glucose levels are generally measured from a tiny blood sample captured from a finger stick test, prior to eating or sleeping. Another critical challenge is accurately estimating how many carbohydrates they eat. These blood sugar readings, along with the amount of carbs eaten, must be interpreted to decide how much insulin the individual needs to inject. Exercise and fitness also impact the amount of insulin required. Continuous blood glucose monitors are available on the market, but are not yet as accurate as finger sticks tests. There are many judgment calls and best guesses being made on a daily basis by individuals with Type 1 diabetes. And though medical technology for diabetes is very advanced and reliable, he is working on an artificial pancreas that would remove the need for most of this guesswork.”
 HbA1C Results Prove Inaccurate For Dialysis Patients: According to a new study at Wake Forest Baptist Medical Center, a test known as the golden standard long-term glucose monitoring test proved to be less valuable in patients who are on dialysis.
HbA1C Results Prove Inaccurate For Dialysis Patients: According to a new study at Wake Forest Baptist Medical Center, a test known as the golden standard long-term glucose monitoring test proved to be less valuable in patients who are on dialysis. Master Gene Found To Cause Obesity And Diabetes: According to a study led by a team of King’s College London and the University of Oxford researchers, a “master regulator” gene is being named the culprit of high cholesterol levels and type 2 diabetes in the body.
Master Gene Found To Cause Obesity And Diabetes: According to a study led by a team of King’s College London and the University of Oxford researchers, a “master regulator” gene is being named the culprit of high cholesterol levels and type 2 diabetes in the body. New System Could Convert Cells Into Making
New System Could Convert Cells Into Making 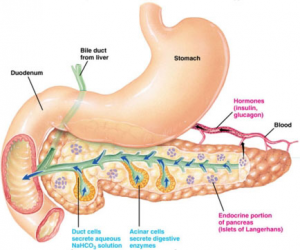
 Clinical Trial Finds Weight Loss Through An Experimental Drug: Researchers at Duke University Medical Center have found that an investigational combination of drugs that are used to treat epilepsy, migraine and obesity is producing a 10 percent weight loss in patients who were suffering from obesity during a one-year clinical trial.
Clinical Trial Finds Weight Loss Through An Experimental Drug: Researchers at Duke University Medical Center have found that an investigational combination of drugs that are used to treat epilepsy, migraine and obesity is producing a 10 percent weight loss in patients who were suffering from obesity during a one-year clinical trial. Possible New Non-Insulin Treatment Found For Type 1 Diabetes: While Type 2 diabetes is more common, many patients find themselves becoming diagnosed with Type 1 diabetes. Through-out many years, Type 2 diabetic patients have been placed on a strict diet and exercise regime while patients with Type 1 diabetes are often treated with
Possible New Non-Insulin Treatment Found For Type 1 Diabetes: While Type 2 diabetes is more common, many patients find themselves becoming diagnosed with Type 1 diabetes. Through-out many years, Type 2 diabetic patients have been placed on a strict diet and exercise regime while patients with Type 1 diabetes are often treated with 
 Research Shows Safflower Oil Helping Type 2 Diabetics: Safflower oil, which can be found in many kitchens around the world, is finding its name on headlines this week. Thanks to a recent study, a person who takes a daily dose of safflower oil for 16 weeks can improve cholesterol levels,
Research Shows Safflower Oil Helping Type 2 Diabetics: Safflower oil, which can be found in many kitchens around the world, is finding its name on headlines this week. Thanks to a recent study, a person who takes a daily dose of safflower oil for 16 weeks can improve cholesterol levels,