 Lab-Created Blood Vessels Helping Dialysis Patients: Imagine having to stop your kidney dialysis because your veins are shot? Just kaput, not one viable vein.
Lab-Created Blood Vessels Helping Dialysis Patients: Imagine having to stop your kidney dialysis because your veins are shot? Just kaput, not one viable vein.
Then imagine a refrigerated room stockpiled with lab-created blood vessels where one can walk into the room and pick out a blood vessel that is going to fit the recipient who is in dire need of a vein to help with their kidney dialysis, help with their heart bypass surgery, help with their poor circulation in their limbs and help in any other way where a blood vessel needs to be replaced. These new blood vessels would be created without the use of artificial materials, and no stem cells would be involved in their creation.
The works are set in place to create this imaginary refrigerated room to store those newly grown blood vessels. Just think of the ease this would provide in a medical crisis where a call could simply be placed for the type blood vessel that might be needed, and the blood vessel could be sent to the OR as easily as the request is now made for a pacemaker.
The process for growing these new, straw-shaped blood vessels involves taking a snippet of skin from the back of a hand, removing cells and then growing them into a sheet of tissue that can be rolled up like drinking straws to form blood vessels.
Recently in Poland, three patients received such new blood vessels for health issues, and those vessels are still working two to eight months later. Those blood vessels that the patients in Poland received were blood vessels that were grown in a lab using donated skin.
The potential for lab-created vessels will be a lifesaver for many people. The process is in its earliest stages, but further testing is ongoing in Europe and South America on a larger scale, and the hope is that the results from these larger test studies will prove just as favorable.
This could prove to be a medical miracle for those in need of blood vessel replacement.
Blood vessels/veins are needed in so many areas of the medical field. Many diabetics have kidney failure as a result of long-term diabetes. Right now, approximately 400,000 Americans undergo kidney dialysis. When kidneys fail, a person must have kidney dialysis or they will die. Kidney dialysis involves artificially filtering the waste from the blood through a connection between the artery and a vein. This connection is called a shunt. This shunt gets poked numerous times a week in order to hook the patients up to the dialysis machine. There are many complications that can arise with the shunt – blood clots, infection and even clogging. As well, this shunt has to be inserted into a vein. Eventually, some patients run out of viable blood veins for their dialysis requirements. If a person could have a new vein inserted, this could extend the length of time they are on dialysis until a kidney transplant could become an option.
Thousands and thousands of people undergo open heart surgery each year. Think of the celebrities we hear about in the news – David Letterman, Regis Philbin, Star Jones, Barbara Walters, Robin Williams, Burt Reynolds, and many, many more. There are people you pass on the street everyday who have undergone the same process.
In fact, approximately 300,000 people a year have heart bypass operations wherein veins are removed from their legs and are used to replace the clogged arteries in their hearts. In many cases, the wound on the leg from the removal of the vein is difficult to heal and has to be watched closely for infection. If a straw-shaped, lab-created blood vessel could be used from this stockpile of blood vessels there would be no need for the surgical removal of the vessel in the leg for use in the heart.
Thus far, these straw-shaped, lab-grown blood vessels have been well tolerated by the patients who received them, so much so that there was no need for anti-rejection medication and tissue matching was not necessary.
At the present time, lab-grown skin is already used to treat many burn victims. This creation of the blood vessels in a lab is a giant step forward for the medical field.
 Oakland A’s, MUG Root Beer and Juvenile Diabetes: The Oakland A’s held their annual MUG Root Beer Float Day event on June 30, 2011, at the East Side Club at the Coliseum in Oakland, California. All proceeds from this event went to the Juvenile Diabetes Research Foundation to help in the search for a cure for diabetes and its
Oakland A’s, MUG Root Beer and Juvenile Diabetes: The Oakland A’s held their annual MUG Root Beer Float Day event on June 30, 2011, at the East Side Club at the Coliseum in Oakland, California. All proceeds from this event went to the Juvenile Diabetes Research Foundation to help in the search for a cure for diabetes and its  600 Calories Per Day A Cure For Type 2: Don’t even think about trying such a drastic diet. If you are attempting to
600 Calories Per Day A Cure For Type 2: Don’t even think about trying such a drastic diet. If you are attempting to  7 Year Old Sydney Lyons, Congress and Diabetes: In June 2011, little Sydney Lyons of Pocatello, Idaho, testified before the Children’s Congress of the United States in Washington, D.C., on behalf of the Juvenile Diabetes Research Foundation and was also able to speak to the Congressional Diabetes Caucus. Sydney has Type 1 diabetes and was before Congress to talk about funding more research for Type 1 diabetes so a cure can be found.
7 Year Old Sydney Lyons, Congress and Diabetes: In June 2011, little Sydney Lyons of Pocatello, Idaho, testified before the Children’s Congress of the United States in Washington, D.C., on behalf of the Juvenile Diabetes Research Foundation and was also able to speak to the Congressional Diabetes Caucus. Sydney has Type 1 diabetes and was before Congress to talk about funding more research for Type 1 diabetes so a cure can be found. Study on Liraglutide (Victoza) Could Help Type 1 Diabetics: The University of Buffalo conducted an observation study in regards to the use of liraglutide, an injectable
Study on Liraglutide (Victoza) Could Help Type 1 Diabetics: The University of Buffalo conducted an observation study in regards to the use of liraglutide, an injectable  Can eating 37 strawberries a day lessen diabetes
Can eating 37 strawberries a day lessen diabetes  Tom Martinez, Facebook And A Donor: Back in June of 2011, famous quarterback coach Tom Martinez announced on his Facebook page that his
Tom Martinez, Facebook And A Donor: Back in June of 2011, famous quarterback coach Tom Martinez announced on his Facebook page that his 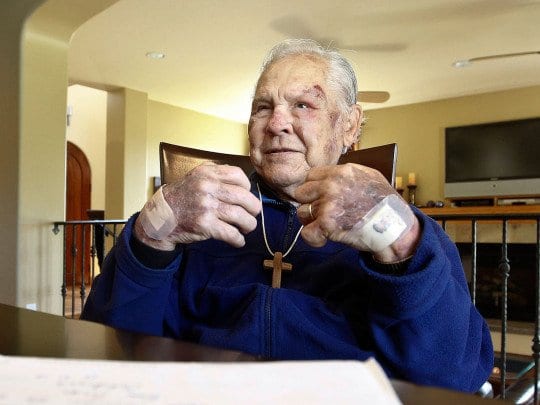
 New Discoveries Made in Conquering
New Discoveries Made in Conquering  High-Fat Diet
High-Fat Diet