 Body Muscle Mass Helps Fight Insulin Resistance: Body muscle mass helps prevent insulin resistance even in overweight individuals. Insulin resistance, in many cases, leads to a diagnosis of type 2 diabetes. There is a possibility of stopping the progression from a diagnosis of insulin resistance to full-blown type 2 diabetes with building additional body muscle mass. Insulin resistance is a condition where blood glucose levels are higher than the normal range and is a cause for concern in one’s overall health.
Body Muscle Mass Helps Fight Insulin Resistance: Body muscle mass helps prevent insulin resistance even in overweight individuals. Insulin resistance, in many cases, leads to a diagnosis of type 2 diabetes. There is a possibility of stopping the progression from a diagnosis of insulin resistance to full-blown type 2 diabetes with building additional body muscle mass. Insulin resistance is a condition where blood glucose levels are higher than the normal range and is a cause for concern in one’s overall health.
A recent study, the results of which are soon to be published in The Endocrine Society’s Journal of Clinical Endocrinology and Metabolism, was recently done at the University of California, Los Angeles. The senior author of the study results, Preethi Srikanthan, M.D., stated, “Our findings represent a departure from the usual focus of clinicians, and their patients, on just losing weight to improve metabolic health.” Srikanthan further added, “Instead, this research suggests a role for maintaining fitness and building muscle. This is a welcome message for many overweight patients who experience difficulty in achieving weight loss, as any effort to get moving and keep fit should be seen as laudable and contributing to metabolic change.”
In studies in the past, it was discovered that low muscle mass is a risk factor for insulin resistance. Until this time, however, no study had examined whether increasing the body muscle mass to average and then above average levels, separately from the overall body weight, would lead to improved blood sugar levels.
This study took into account the body muscle mass in relationship to insulin resistance and blood sugar metabolism disorders. It was a nationally representative group sample of 13,644 people. Those in the study were all older than 20 years of age, none were expecting a child and they all weighed more than a set figure. This study reflected that the more muscle mass an individual had in relationship to body size the less likely the individual was to insulin sensitivity and, therefore, a lower risk of pre-diabetes.
Usually, research has indicated that individuals with a waist circumference within certain inches is a good indicator for pre-diabetes – the larger the waist measurement, the more likely an individual is to develop pre-diabetes or even diabetes. Body mass index has been taken into account as well.
Dr. Srikanthan added, “Our research shows that beyond monitoring changes in waist circumference or BMI, we should also be monitoring muscle mass.”
More research would be needed to determine how much help can be garnered from intervention in a person’s life in regards to their exercise routine, to include lightweight weights and more cardio exercise.
Simply lifting soup cans in a repetitive manner (arm curls or over the head) while standing in the kitchen can benefit anyone. As well, doing small push-ups from the kitchen counter can strengthen the arms. Doing ten lunges when dusting can strengthen the leg muscles. Small changes can be incorporated into an individual’s daily life that would help tone and build muscle mass. In the process, an individual could be helping to prevent the diagnosis of pre-diabetes or even full-blow diabetes.
 Cell Phones Helping Manage Diabetes: According to a new study from the University Of Maryland School Of Medicine, an interactive computer software program could be very effective in helping patients with type 2 diabetes, manage their diabetes using their mobile phone.
Cell Phones Helping Manage Diabetes: According to a new study from the University Of Maryland School Of Medicine, an interactive computer software program could be very effective in helping patients with type 2 diabetes, manage their diabetes using their mobile phone. New Research – Stem Cell Memory and
New Research – Stem Cell Memory and  No Higher Risk for Type 2 Diabetes In Natural Menopause versus Ovarian Removal Menopause: Whether menopause comes naturally as a female ages or is brought on at an earlier age due to a hysterectomy that involves ovary removal, there is no increase in the diagnosis of type 2 diabetes, and the risk for type 2 diabetes does not increase.
No Higher Risk for Type 2 Diabetes In Natural Menopause versus Ovarian Removal Menopause: Whether menopause comes naturally as a female ages or is brought on at an earlier age due to a hysterectomy that involves ovary removal, there is no increase in the diagnosis of type 2 diabetes, and the risk for type 2 diabetes does not increase. V-Go Disposable
V-Go Disposable 
 Diabetes Cure:
Diabetes Cure: 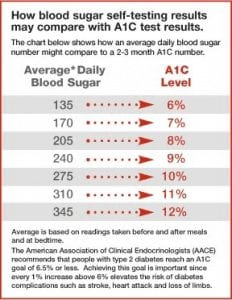 Is Tight Blood Sugar Controls Best for Type 2 Diabetes: Should persons with type 2 diabetes keep their blood sugar levels under strict control, resulting in their
Is Tight Blood Sugar Controls Best for Type 2 Diabetes: Should persons with type 2 diabetes keep their blood sugar levels under strict control, resulting in their  Diagnosing Diabetes and
Diagnosing Diabetes and  Nuts Over Carbs for Diabetes: A recent study shows that when those dealing with type 2 diabetes switched out some of their regular carbohydrates for a half cup of mixed nuts each day, the participants’ blood sugar levels and LDL cholesterol levels dipped slightly over three months. This is no reason to eat nuts all day long, but it’s a good enough reason to think about throwing in some nuts in place of the carbs each day.
Nuts Over Carbs for Diabetes: A recent study shows that when those dealing with type 2 diabetes switched out some of their regular carbohydrates for a half cup of mixed nuts each day, the participants’ blood sugar levels and LDL cholesterol levels dipped slightly over three months. This is no reason to eat nuts all day long, but it’s a good enough reason to think about throwing in some nuts in place of the carbs each day.