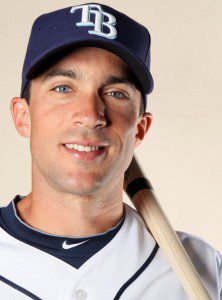
 Tampa Bay Rays outfielder Sam Fuld made the day of one six-year-old boy when he visited Andrew Cordovez in an examination room. Fuld had one special connection with the young boy: they both have Type 1 diabetes.
Tampa Bay Rays outfielder Sam Fuld made the day of one six-year-old boy when he visited Andrew Cordovez in an examination room. Fuld had one special connection with the young boy: they both have Type 1 diabetes.
Andrew received an autograph picture of Fuld and a baseball. “That was cool,” said Andrew. “He’s a really good player.”
Fuld visited the newly-founded diabetes center at the University of South Florida, taking a two-hour tour of the 10,000 square foot facility. The diabetes center, which opened last month, is part of the Carol & Frank Morsani Center for Advanced Healthcare.
Officials at the University of South Florida hope that the facility will propel them to the forefront of research, education and treatment of diabetes. The disease affects more than 23 million people around the country.
According to the dean of the USF College of Medicine, Dr. Stephen Klasko, the university is quickly becoming a national leader in diabetes research. The university has received more than $400 million for its efforts in studying diabetes but did not have a clinical facility. The new diabetes center cost $2 million; university funds and donations paid for the facility.
Facility officials who met Fuld included Dr. Klasko, Judy Genshaft (USF President) and Drs. Jeffrey Krischer and Henry Rodriguez (heads of the new center). The group all wore Tampa Bay jerseys.
Fuld visited the center with wife, Sarah, and son, Charlie, in tow. Charlie is 20 months old and does not have diabetes but his parents are wary since the disease is hereditary and Charlie is at increased risk.
“It’s a cause near and dear to my heart,” said Fuld of diabetes. He was diagnosed with Type 1 diabetes at only 10 years old. But like Andrew Cordovez, Fuld was visited by an athlete with Type 1 diabetes when as a young boy. Fuld met Bill Gullickson, a professional pitcher who also had Type 1 diabetes, when Fuld was 12 years old.
Gullickson had encouraging words for Fuld. “He told me I could do anything, academically and athletically, I wanted to,” said Fuld of the meeting.
Fuld took the advice to heart and made the best of his situation. Now 29 years old and known as “Super Sam,” Fuld’s athletic style of fielding has garnered attention and adoration from fans. His athleticism belies the fact that his diabetes requires him to perform regular blood sugar checks on himself, six to seven times a day, including two to three times in the middle of games. Fuld also administers his own insulin shots four to five times every day. “I keep those up in the clubhouse in the locker room. So if you see me running up the tunnel to go to the locker room, that’s probably why,” said Fuld.
According to Fuld, he has an advantage in that baseball is more flexible in addressing his diabetes. “All that down time in the dugout. So I get plenty of time to check my sugar. And I give myself shots probably four to five times a day.”
“My outlook on it, all along was just look at it as a challenge,” Fuld said of living with diabetes.
Fuld isn’t the only athlete who achieved success despite being diagnosed with diabetes. Other diabetic athletes include NFL quarterback Jay Cutler, Indy car driver Charlie Kimball, Olympic gold medalist swimmer Gary Hall Jr. and two tennis Hall of Famers: Billie Jean King and Arthur Ashe.
 Mannkind (MKND) stock rose more than 20%, showing increased investor confidence after the fledgling pharmaceutical company confirmed that it has received approval from the FDA for clinical trials on its key product. Mannkind received FDA clearance to conduct efficacy trials on a new inhaled
Mannkind (MKND) stock rose more than 20%, showing increased investor confidence after the fledgling pharmaceutical company confirmed that it has received approval from the FDA for clinical trials on its key product. Mannkind received FDA clearance to conduct efficacy trials on a new inhaled  Researchers at York University have discovered a new
Researchers at York University have discovered a new  Patients suffering with Type 2 diabetes are commonly prescribed a combination of
Patients suffering with Type 2 diabetes are commonly prescribed a combination of  Fat Levels Higher in Thin Children” width=”290″ height=”249″ />A study conducted by Children’s Hospital Boston and the Joslin Diabetes Center has revealed that levels of “brown fat,” a healthy type of fat that appears in children, increase in puberty and then decrease after. The study also showed that thinner children have higher levels of brown fat. The study was published in the Journal of Pediatrics.
Fat Levels Higher in Thin Children” width=”290″ height=”249″ />A study conducted by Children’s Hospital Boston and the Joslin Diabetes Center has revealed that levels of “brown fat,” a healthy type of fat that appears in children, increase in puberty and then decrease after. The study also showed that thinner children have higher levels of brown fat. The study was published in the Journal of Pediatrics. The Journal of Sexual Medicine recently published a new study demonstrating that weight loss in men with Type 2 diabetes is more than just a healthy choice. It also improves sexual health, increasing erectile function and desire while lowering the risk of developing urinary tract symptoms.
The Journal of Sexual Medicine recently published a new study demonstrating that weight loss in men with Type 2 diabetes is more than just a healthy choice. It also improves sexual health, increasing erectile function and desire while lowering the risk of developing urinary tract symptoms. The smell of that hamburger or steak (unprocessed meat) on the backyard grill is tantalizing, but we all know that we’re not supposed to have too much of it simply because it’s not great for our health for a number of reasons, to include the susceptibility to type 2 diabetes. But, it’s now known that that hotdog (processed meat) lying beside that hamburger on the grill might be a little bit worse for your health than the burger or steak, including your susceptibility to type 2 diabetes.
The smell of that hamburger or steak (unprocessed meat) on the backyard grill is tantalizing, but we all know that we’re not supposed to have too much of it simply because it’s not great for our health for a number of reasons, to include the susceptibility to type 2 diabetes. But, it’s now known that that hotdog (processed meat) lying beside that hamburger on the grill might be a little bit worse for your health than the burger or steak, including your susceptibility to type 2 diabetes. The heavy competition present in the modern
The heavy competition present in the modern  Boston Therapeutics has filed an abbreviated new drug application (or ANDA) with the Food and Drug Administration. The new drug appears in the form of chewable
Boston Therapeutics has filed an abbreviated new drug application (or ANDA) with the Food and Drug Administration. The new drug appears in the form of chewable 