Kondrake Calls For a Diabetic War: Morton Kondrake is quoted as saying, “One’s dignity may be assaulted, vandalized and cruelly mocked, but it cannot be taken away unless it is surrendered.” So when he recently took on the subject of diabetes we paid attention to a man who seems to understand the concept of dignity.
Kondrake is a journalist and writer for the non-partisan Capitol Hill newspaper, “Roll Call”. His recent piece was entitled, “Kondracke: Declare war on diabetes”.
Here are some highlights.
“The reason for a war on diabetes is that, like some cancers, Type 2 diabetes – the most prevalent type – is heavily a “lifestyle disease” resulting from overeating and lack of activity. Therefore, it’s preventable.”
“Diabetes can result in ghastly consequences for its 24 million victims, including heart disease, stroke, blindness, kidney failure, amputations and nervous system disease, and it is hugely expensive to the economy.”
“Nineteen different federal agencies spent only $3.9 billion on disease-prevention or health-promotion activities with some impact on diabetes.”
“If a ‘war on diabetes’ were declared, it ought to begin with a war on obesity, the epidemic most responsible for rising incidence of Type 2 diabetes among both adults and, increasingly, children.”
“Fighting obesity ought to be a major focus of health care reform.”
“Obesity costs – as much as 27 percent of recent increases in national health spending, according to health analyst Kenneth Thorpe.”
“There’s a need for better diabetes screening in government health programs. Medicaid and Medicare ought to adopt the kind of intensive disease-management techniques that many insurance plans employ.”
“The Congressional Budget Office estimates costs and savings only within a 10-year ‘window,’ whereas chronic-disease management probably would show results over a longer period.”
“A new study in the journal Health Affairs estimated that what amounts to a ‘war’ on diabetes, costing $800 million a year, would merely pay for itself over 25 years, not cut the actual costs to the government.”
“Such a war surely would prevent many strokes, heart attacks, leg amputations and kidney failures. It’s hard to believe that wouldn’t save money, too.”
Kondrake is an advocate of providing some rather graphic video footage of what some diabetics may experience in an effort to shock teens into making better choices in food and lifestyle.
The ‘war’ on diabetes must always come back to one fighter – the individual. Kondrake’s comments seemed especially targeted at preventable Type 2 diabetes and not Type 1 where development is not contingent on lifestyle choices.
Most health professionals would welcome extra funding to help in educational endeavors as well as prevention techniques and mentoring. Kondrake indicates a strong inclination that the government itself makes some beneficial advances more difficult. He cites testing equipment specifically. In Asian countries for example there is testing equipment that can be used to wirelessly send data to a computer for tracking. Such devices would need approval from the Food and Drug Administration (FDA) every time the device is altered for technological reasons in the U.S.
The battle for funding continues for organizations that have waged their own war on diabetes. The good news is that as you read through this site you will discover a multitude of new studies offering promise and hope. You will read of individuals who have managed their own personal battles and are holding the line. While there is hope that more help will come, the responsibility for our health often rests squarely with us. So, we keep working to provide information you can use to fight. Together perhaps we will one day win.
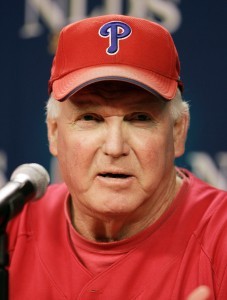 Phillies Manager on His Own Diabetes Win Streak: Charlie Manuel is a big man, and he took a big team to the World Series in 2008. The Phillies manager guided his team to an incredible year, but excessive weight and Type 2 diabetes found him on a collision course with disaster.
Phillies Manager on His Own Diabetes Win Streak: Charlie Manuel is a big man, and he took a big team to the World Series in 2008. The Phillies manager guided his team to an incredible year, but excessive weight and Type 2 diabetes found him on a collision course with disaster.