The crew aboard the Apollo 13 discovered a “Main B bus undervolt.” I don’t have to know what that means to understand that when astronaut John Swigert, Jr. said, “Houston, we’ve had a problem,” he meant every word.
Mayo’s New Diabetes Reference Guide: The crew aboard the Apollo 13 discovered a “Main B bus undervolt.” I don’t have to know what that means to understand that when astronaut John Swigert, Jr. said, “Houston, we’ve had a problem,” he meant every word.
Today the phrase has been recast to “Houston we have a problem” and the line has become a bit cliché, but it remains a strong reminder that when the words are uttered there are difficulties being faced.
In their own way the Mayo Clinic has uttered those words – and they were directed toward all of us in response to the epidemic that is diabetes.
A Voice Of America report quotes Dr. Maria Collazo-Clavell of the Mayo Clinic as saying, “Probably the No. 1 cause of diabetes becoming so common, [as well as] pre-diabetes, is definitely our lifestyle. Most of us are heavier than we have been in the past and less active. So definitely being conscious about our eating habits, weight and activity become very important to preventing type 2 diabetes, particularly.”
Collazo-Clavell is the medical editor for a new manual called the Essential Diabetes Book. It has been described by VOA as a, “Comprehensive and up-to-date manual on diabetes, intended for the general public.”
The book asserts that there are twice as many pre-diabetics as there are those who have actually been diagnosed with the disease. Pre-diabetes has been described as a condition where, “Blood glucose levels are higher than normal, but not high enough for a type 2 diabetes diagnosis. Pre-diabetes is also dangerous because long-term damage to the heart and circulatory system might already have begun to occur.”
The book touches on diabetes as it relates to various ethnicities. For example Type 1 diabetes is more common among Caucasian youth while Type 2 is more prevalent among African American and Hispanic adults. As we’ve reported here before another primary concern for diabetics is being able to access healthy meals and exercise is often difficult to manage due to the fact that diabetes can make an individual feel very tired.
However Collazo-Clavell suggests, “Whatever physical activity someone can do, it is worth doing. What often happen is that people have so many other limitations that keep them from adhering to this perfect, beautiful 30- to 45-minute program that they are supposed to do four to five times per week. But what we learned is that short bouts of activity are just as helpful as prolonged bouts of activity.”
You may remember a recent report here that indicates short bursts of intense physical exercise may do more to flood blood sugar from your body that longer, but less intense exercise.
Collazo-Clavell even commented on President Obama’s recent decision to allow embryonic stem cell research. “Once you accomplish, for example, stem cells that can produce insulin and that are viable, often the application to a diverse population of patients becomes quite challenging. So I still feel that we have to focus on helping our patients manage their diabetes day in and day out and not wait for that cure that we have been waiting for for a long time.” The VOA report indicates she does not expect any breakthroughs from embryonic stem cell research anytime soon.
The hard cover book, Essential Diabetes Book is available for around $25 or less and provides a comprehensive look at Diabetes and it’s long-term care.
Offering her own encouragement Collazo-Clavell adds, “”It is never too late to start caring for your health and protecting your health, but the sooner somebody does it, the better a life they will lead.”
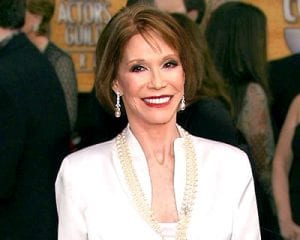 Mary Tyler Moore Speaks Out on Diabetes: “Chronic disease, like a troublesome relative, is something you can learn to manage but never quite escape. And while each and every person who has type 1 prays for a cure, and would give anything to stop thinking about it for just a year, a month, a week, a day even, the ironic truth is that only when you own it–accept it, embrace it, make it your own–do you start to be free of many of its emotional and physical burdens.” That’s how Mary Tyler Moore started her new book, Growing Up Again: Life, Loves, and Oh Yeah, Diabetes.
Mary Tyler Moore Speaks Out on Diabetes: “Chronic disease, like a troublesome relative, is something you can learn to manage but never quite escape. And while each and every person who has type 1 prays for a cure, and would give anything to stop thinking about it for just a year, a month, a week, a day even, the ironic truth is that only when you own it–accept it, embrace it, make it your own–do you start to be free of many of its emotional and physical burdens.” That’s how Mary Tyler Moore started her new book, Growing Up Again: Life, Loves, and Oh Yeah, Diabetes.