 A study conducted by researchers at Kaiser Permanente shows that those with Type 2 diabetes would be wise to work at improving their cholesterol. According to the findings of the study, raising HDL cholesterol — or “good” cholesterol — could be associated with a reduction in the risk of stroke and heart disease in Type 2 diabetics. The study was published in the online version of the “American Journal of Cardiology.”
A study conducted by researchers at Kaiser Permanente shows that those with Type 2 diabetes would be wise to work at improving their cholesterol. According to the findings of the study, raising HDL cholesterol — or “good” cholesterol — could be associated with a reduction in the risk of stroke and heart disease in Type 2 diabetics. The study was published in the online version of the “American Journal of Cardiology.”
Researchers arrived at their findings after reviewing medical records from 30,067 patients with Type 2 diabetes. The patients had their HDL cholesterol levels measured twice over a time period from 2001 to 2006, with the measurements being conducted from six to 24 months apart. The research team analyzed the records and reviewed the data for hospitalization due to heart disease and stroke among the patients. Then they compared HDL cholesterol data to determine whether those who improved their cholesterol between the two measurements saw any difference in hospitalization rates.
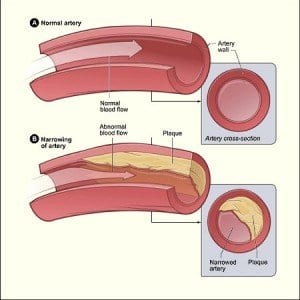
The researchers discovered that, for every 5mg/dL rise in HDL cholesterol, the patients reduced their risk of hospitalization due to heart disease or stroke by 4 percent. Additionally, an increase in HDL of 6.5mg/dL or more was associated with an 11 percent decrease in risk of hospitalization. According to the researchers, this demonstrated “that the prevention of a HDL cholesterol decrease might be at least as important as increasing the HDL cholesterol level.”
About half of all people who have been diagnosed with Type 2 diabetes also have low HDL levels, which are defined as below 40mg/dL for men and below 50mg/dL for women. According to the National Cholesterol Education Program, which is associated with the National Heart, Lung, and Blood Institute, an HDL cholesterol level of under 40mg/dL is considered to be a risk factor for heart disease and stroke.
However, the researchers at Kaiser Permanante noted that studies have still not shown that increasing HDL cholesterol levels causes a direct decrease in risk of heart attack and stroke, “perhaps because safe and effective agents that substantially increase the HDL cholesterol level remain elusive.”
According to Suma Vupputuri, investigator at the Kaiser Permanente Health Research Center in Atlanta, one possible limitation of the study is that researchers did not have access to information about what the patients did to increase their HDL cholesterol levels. It is known that lifestyle changes such as regular exercise, weight loss, and avoiding tobacco can have a positive effect on HDL. However, those changes are also known to reduce the chances of cardiovascular disease; as such, it’s unclear whether the increase in HDL or the improved lifestyles are the main catalyst behind lower risk of hospitalization.
Whether it’s improved HDL cholesterol or lifestyle changes that lead to the lower risk of hospitalization, patients are benefited either way. “I think the general message, certainly, from our paper, is yes, raising HDL is going to improve your cardiovascular outcomes,” said Vupputuri.
Steven Grover, M.D., M.P.A., director of the Cardiovascular Improvement Program at McGill University, agrees that improving HDL reduces the risk of hospitalization. “There’s enough supportive evidence from clinical trials that there’s good reason to believe raising HDL will work” to reduce that risk. Grover conducted a study in 2009 that demonstrated similar benefits in raising HDL cholesterol; however, his findings showed even greater benefits.