 In addition to Type 1 and Type 2 diabetes, there is another variant of the disease: cystic fibrosis-related diabetes. It differs in some important ways from Type 1 and Type 2 diabetes and it requires different treatment methods.
In addition to Type 1 and Type 2 diabetes, there is another variant of the disease: cystic fibrosis-related diabetes. It differs in some important ways from Type 1 and Type 2 diabetes and it requires different treatment methods.
Patients with cystic fibrosis experience decreased nutritional and pulmonary health several years before they’re diagnosed with cystic fibrosis-related diabetes (CFRD). According to Amanda Leonard, a senior pediatric clinical dietician at the Johns Hopkins Cystic Fibrosis Center, early diagnosis and treatment can significantly improve life expectancy in patients who develop CFRD.
“Screening early and knowing which patients are at risk is really important,” said Leonard at a pediatric nutrition meeting sponsored by Johns Hopkins University.
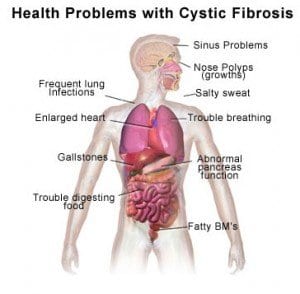
CFRD does “share some components” with Type 1 and Type 2 diabetes, says Leonard, but it’s also different in some important ways. Patients with CFRD typically experience decline in lung function, protein catabolism, weight loss, and an increased rate of mortality. Ketones rarely appear in patients with CFRD, and the development of the disease does not appear to be related to autoimmune function.
In cystic fibrosis patients at the age of 40, the rate of CFRD is over 50 percent. According to Leonard, more patients develop CFRD in the 20-24 year old range than any other age; meanwhile, Type 1 diabetes usually develops in childhood and Type 2 diabetes usually develops in mid-to-late adulthood.
“In CFRD there is a severe insulin deficiency, but it’s not as complete as in type 1,” said Leonard. Physicians define CFRD as the presence of at least two of the following criteria on at least two occasions: hemoglobin A1c of at least 6.5 percent; fasting glucose level of at least 126 mg/dL; and a two-hour oral glucose tolerance test of plasma glucose at least 200 mg/dL.
Leonard says that CFRD isn’t quite as easy to identify as other types of diabetes. In patients with CFRD, a two-hour oral glucose tolerance test (OGTT) can range from 140 to 199 mg/dL while fasting glucose can range from 100 to 125 mg/dL. According to Leonard, it’s “not quite diabetes, but it’s not quite right either.” The disease is “not an all or nothing kind of thing. It’s not that either you have it or you don’t. It can be transient in nature, and there’s a spectrum,” she continued.
Outpatient OGTTs are the best option for routine CFRD testing in clinically stable patients. Cystic fibrosis patients are recommended to begin OGTT screening for diabetes when they reach 10 years of age.
While HbA1c alone cannot be used as to screen for CFRD due to a high rate of false positives, a low HbA1c can confirm a diagnosis from other symptoms.
Patients who are hospitalized due to pulmonary exacerbation and/or treatment with corticosteroids should be tested with both fasting and two-hour post-meal blood glucose monitoring. The patient is diagnosed with CFRD when fasting or post-meal hyperglycemia lasts longer than 48 hours.
Patients with CFRD are treated with insulin; other treatment methods have not shown benefits for patients and are not recommended over insulin. “Insulin is the treatment of choice. Oral agents do not seem to work as well,” said Leonard.
CFRD patients have the same blood glucose goals as other diabetes patients, with an HbA1c goal of less than 7.0 percent. However, goals are adjusted for each individual patient.
Nutritional recommendations for patients with CFRD are based on those for patients with cystic fibrosis. CFRD patients may also benefit from counting carbohydrates to ensure safe blood glucose levels.